Why Should Patients Consider DualPortGYN Procedures Versus Robotic or Standard Laparoscopy?
Why Should Patients Consider DualPortGYN Procedures Versus Robotic or Standard Laparoscopy?
The most important part of the performance of any surgery has to do with the surgeon performing it, and the techniques used.
The Surgeon.
CIGC surgeons are fellowship trained advanced laparoscopic surgical specialists performing high volumes of surgical GYN procedures. CIGC surgeons are completely immersed in surgery. This means that they dedicate themselves to surgery 100 percent of the time, and are FULL-TIME SURGEONS. OBGYNs in comparison are focused mostly on obstetrics rather than surgery, with obstetrics encompassing 60 to 70 percent of their practice. As part-time surgeons, OBGYNs do not have the time, expertise, additional training, and surgical volume to learn or perform procedures using techniques such as DualPortGYN. As a patient, the surgical expertise, training, and exposure to new and better ways of doing surgery are paramount to decreasing complication rates and enhancing surgical success.
The Technique.
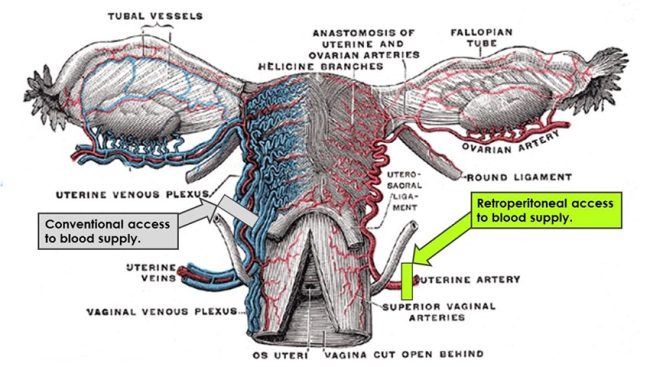
Surgical technique is the most important part of any surgical procedure. Superior techniques lead to superior results. Retroperitoneal approaches to GYN surgery are quickly being recognized by major societies as a better and safer way to perform GYN procedures. So why does the OBGYN not do complete retroperitoneal dissection for their patients? OBGYNs are typically not trained in RP dissection approaches. The focus on obstetrics limits the OBGYN’s ability to learn new approaches to surgery, and their surgical volume is so limited that most only perform one to two major cases a month. The lack of training and low surgical volume do not lend themselves to learning and adopting new and better techniques and approaches to surgery.
The Robot.
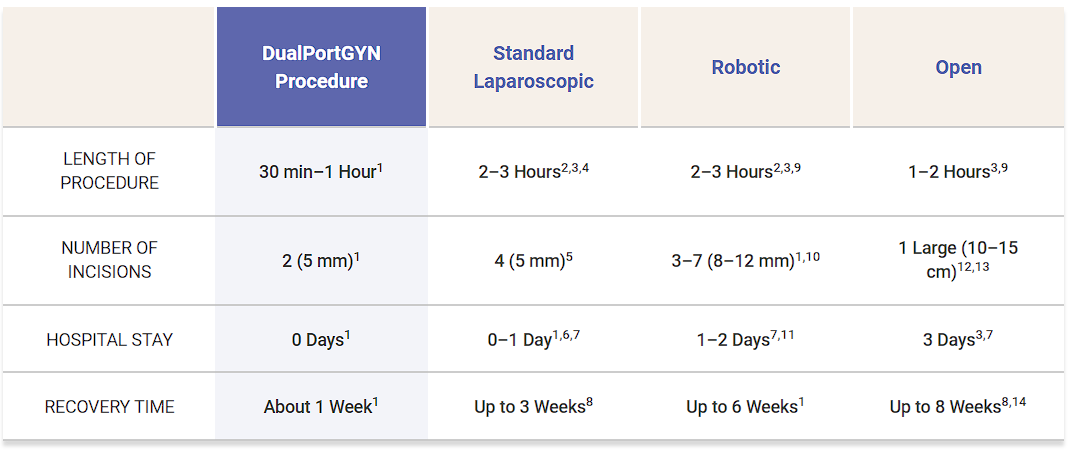
Robotic surgery is only as good as the surgeon sitting behind the console and performing the procedure. Since the robot takes instructions from the surgeon, the robot is only as good as the surgeon directing it. In general, robotics are needed for the OBGYN to perform a type of laparoscopic surgery that has a greater number of incisions, larger incision size, longer surgical times, and higher complication rates than even standard laparoscopy. The robot does not enhance the quality of the surgery, and in actuality may decrease it. There is no substitute for a well-trained surgeon, and the robot is not that substitute.
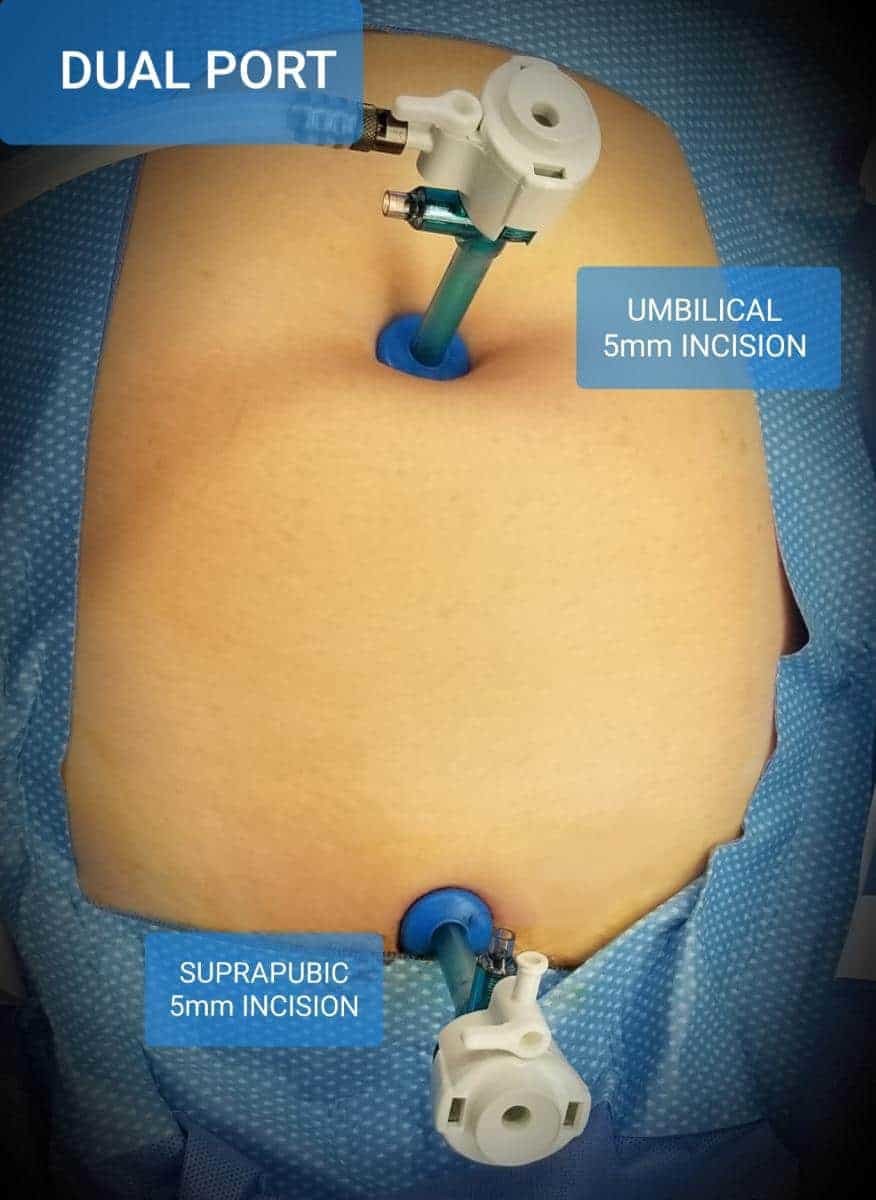
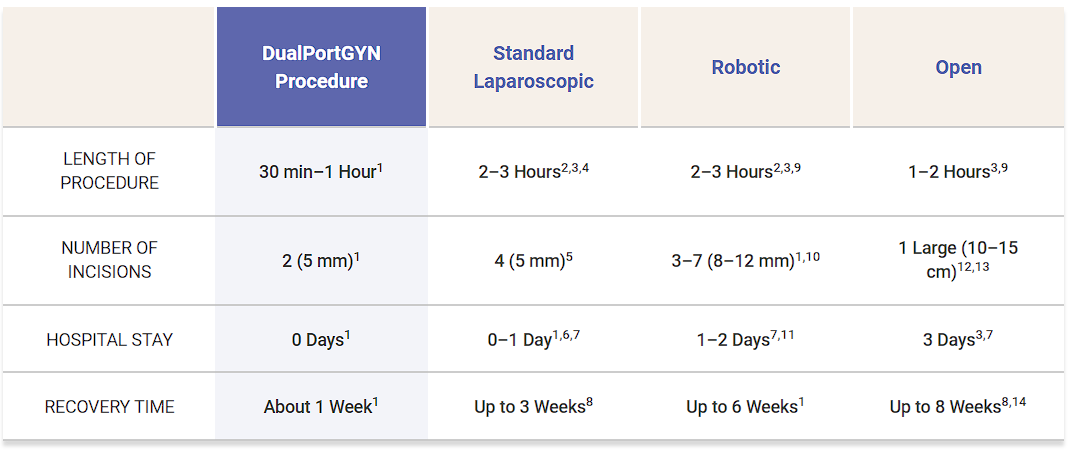
DualPortGYN Compared to Other Surgical Techniques
1 Danilyants N, MacKoul P, Baxi R, van der Does LQ, Haworth LR. Value-based assessment of hysterectomy approaches. JOGR. 2018.
2 Pasic et al. Comparing Robot-Assisted with Conventional Laparoscopic Hysterectomy: Impact on Cost and Clinical Outcomes. JMIG. 2010 17 (6): 730-738
3 Landeen LB, Bell MC, Hubert HB, Bennis LY, Knutsen-Larson SS, Seshadri-Kreaden U. Clinical and cost comparisons for hysterectomy via abdominal, standard laparoscopic, vaginal and robot-assisted approaches. South Dakota Medicine 2011; 64(6): 197-199
4 Drahonovsky J., Haakova L., Otcenasek M., Krofta L., Kucera E., and Feyereisl J.: A prospective randomized comparison of vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy, and total laparoscopic hysterectomy in women with benign uterine disease. EJOGRB 2010; 148: pp. 172-176
5 Einarsson, J. I., & Suzuki, Y. (2009). Total laparoscopic hysterectomy: 10 steps toward a successful procedure. Reviews in obstetrics & gynecology, 2(1), 57-64.
6 Paraiso MF, Ridgeway B, Park AJ, et al. A randomized trial comparing conventional and robotically assisted total laparoscopic hysterectomy. AJOG. 2013;208(5):368.e361–367.
7 Wright KN, Jonsdottir GM, Jorgensen S, Shah N, Einarsson JI. Costs and outcomes of abdominal, vaginal, laparoscopic and robotic hysterectomies. JSLS. 2012;16(4):519-24.
8 Aarts JWM, Nieboer TE, Johnson N, Tavender E, Garry R, Mol BWJ, Kluivers KB. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews 2015, Issue 8. Art. No.: CD003677.
9 Schmitt, J. J., Carranza Leon, D. A., Occhino, J. A., Weaver, A. L., Dowdy, S. C., Bakkum-Gamez, J. N., Pasupathy, K. S., Gebhart, J. B. (2017). Determining Optimal Route of Hysterectomy for Benign Indications: Clinical Decision Tree Algorithm. Obstetrics and gynecology, 129(1), 130-138.
10 Mayo Clinic
11 Paraiso MF, Ridgeway B, Park AJ, et al. A randomized trial comparing conventional and robotically assisted total laparoscopic hysterectomy. AJOG. 2013;208(5):368.e361–367.
12 Yeung P, Bolden C et al. Patient Preferences of Cosmesis for Abdominal Incisions in Gynecologic Surgery. JMIG. 2013; 20(1): 79-84
13 Jones, H. W., III, & Rock, J. A. (2015). Te Linde’s operative gynecology (Eleventh edition). Philadelphia: Wolters Kluwer.
14 Royal College of Obstetricians & Gynaecologists, London, UK.
Back to Top