1 Bolnick A, Bolnick J, Diamond MP. Postoperative adhesions as a consequence of pelvic surgery. J Minim Invasive Gynecol. 2015 May-Jun;22(4):549-63
Pelvic adhesions form when scar tissue creates bands between pelvic organs. They can develop after inflammation from complex GYN conditions, like endometriosis or infection, or from previous surgical procedures, including cesarean sections. These adhesions can create a condition called “frozen pelvis,” where the internal organs become stuck together. Scar tissue can be completely asymptomatic and not cause any problems. However, when scar tissue causes infertility, gastrointestinal problems such as bloating or constipation, or pain, then surgical resection needs to be considered.
Pelvic adhesions require advanced GYN surgical expertise. The Center for Innovative GYN Care® (CIGC®) surgical specialists use advanced minimally invasive GYN techniques for pelvic adhesion resection that provide great care and rapid recovery.
Why are resection of pelvic adhesions life changing? When done properly and safely, expertise in the lysis of adhesions, especially to the bowel and ureter, can change a procedure from a large open incision to a minimally invasive one. This has significant ramifications for all patients, in that open surgery causes severe pain, longer recovery time, higher complications, and often prolonged time from work at a significant financial cost. In the video presented in the section below – Resection of Pelvic Adhesions Procedure – the patient had multiple prior surgeries leading to extensive scarring. These procedures were done “open” and the bowel in the video is densely adherent to the abdominal wall where the incision is. This is a common problem after open surgery. The patient here has a pelvic mass that is very adherent to the side of the body and the large vessels. After the bowel is removed from the abdominal wall, the bowel is then removed from the left pelvic sidewall to expose the mass, which can now be safely removed. This type of “lysis of adhesions” is very complex, time consuming, and can in some cases lead to an “unrecognized bowel injury” in which a small nick in the bowel results in spillage of stool in the abdomen, resulting in patients becoming very ill. Lysis of adhesions such as these are always associated with the risk of bowel injury. A skilled laparoscopic surgeon performing these procedures can greatly reduce the risk, although this risk is never eliminated, and patients must understand that this risk exists in any procedure involving extensive lysis of adhesions and the bowel.
Back to TopScar tissue can involve different organs and requires a certain degree of surgical skill to avoid complications. Laparoscopic resection of pelvic adhesions is the preferred method due to less pain, faster recovery, and less risk of new adhesions compared to open surgery. Many surgeons who perform laparoscopy do not have the skills required to effectively and safely take down the pelvic adhesions. In the hands of an inexperienced laparoscopic surgeon, resection of pelvic adhesions will result in a higher risk of conversion to open surgery and injury to organs such as the bowel and bladder.
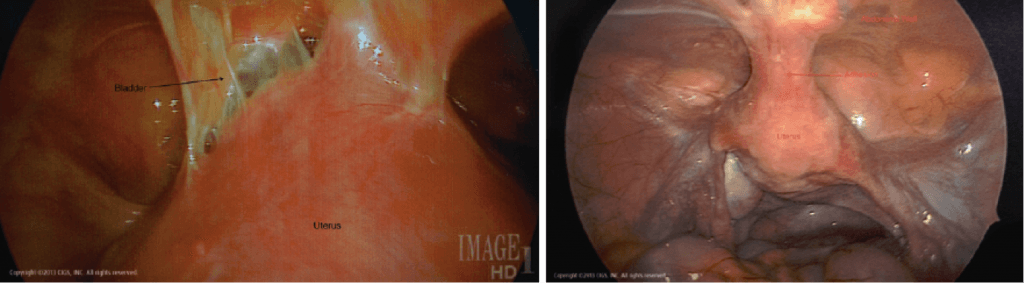
These usually form after cesarean delivery. Multiple cesarean deliveries lead to dense adhesions between the bladder and the uterus. Patients who have had multiple cesarean deliveries should only have an experienced laparoscopic surgeon perform the operation to decrease the risk of bladder injury. To avoid recurrent adhesions and pain, removal of the uterus (hysterectomy) is recommended.
These form after abdominal and pelvic surgeries or severe pelvic infection. After a myomectomy, the bowel can become adherent to the uterus and the abdominal wall. Prior pelvic infection from a ruptured appendix or bowel injury can also lead to severe bowel adhesions. Careful dissection of the bowel with special scissors is required to avoid injury. This procedure should only be performed by an experienced laparoscopic surgeon.
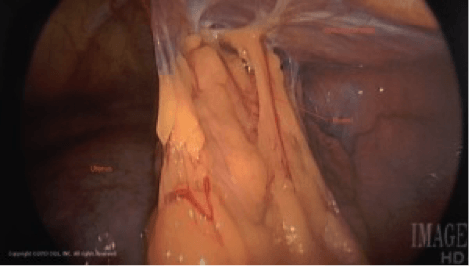
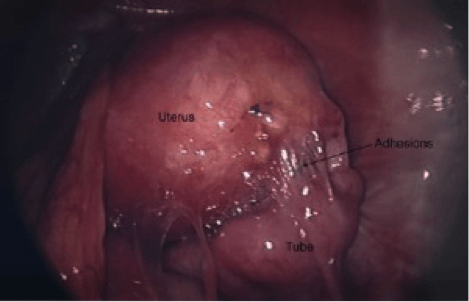
These are the result of longstanding endometriosis and can cause pain and infertility. These adhesions can be very difficult to resect and should only be performed by an experienced laparoscopic surgeon. These adhesions are usually very dense and involve important structures such as the rectum, large pelvic vessels, and ureters. If the patient has completed childbearing, the removal of the uterus with or without the ovaries should be considered to effectively remove the adhesions and resolve pain. If childbearing is desired, careful dissection around the uterus, ovaries, and tubes is performed to avoid bleeding and injury.
These are adhesions around the tubes that connect the kidneys to the bladder. These adhesions are usually found in severe endometriosis. Again, only an experienced surgeon should attempt to take down these adhesions to avoid injury to the ureter. In rare cases, the extent of damage to the ureter from endometriosis requires ureteral reimplantation (ureteroneocystostomy). In this procedure, the damaged segment of the ureter is removed, and the healthy end is implanted directly into the bladder. Very few surgeons are able to perform this procedure laparoscopically, therefore patients with severe endometriosis should seek care from an experienced advanced laparoscopic surgeon.
Back to TopThe DualPortGYN® resection of pelvic adhesion procedure is performed by CIGC laparoscopic GYN surgical specialists with some of the most modern minimally invasive techniques available. The ability to map the pelvis with retroperitoneal (RP) dissection and to control blood loss with uterine artery ligation/occlusion (UAL or UAO) makes it possible to perform advanced procedures efficiently with exceptional results.
RP dissection is an advanced technique used to help laparoscopic GYN specialists visualize and map the pelvic cavity. The retroperitoneal space is covered by a membrane called the peritoneum. By going behind (retro) the lining (peritoneal), the surgeon completely visualizes all of the anatomy of the pelvis including:
This technique is important for the treatment of pelvic scarring that can be extensive in the retroperitoneal space from prior surgery or endometriosis. By visualizing the pelvic cavity, the CIGC surgical specialists can resect adhesions and prevent injuries or complications both during and after the surgery.
Back to TopThe resection of pelvic adhesion procedure requires at least three small incisions that are placed during the course of a procedure to remove or treat a condition. Typically, removal of scar tissue can require extensive time to complete, in many cases longer than the surgery itself. Since this procedure is associated with significant risk, the surgeon performing the removal of the scar tissue must be experienced in the process, and be able to repair injuries to associated structures involved with the scarring. Repair of the bowel, bladder, and other structures may be necessary when scar tissue removal is involved.
Pelvic adhesions often occur after prior surgery or due to infection, endometriosis, or other causes. Adhesions increase the risk of the surgical procedure since they can densely “stick together” vital structures so that normal anatomy cannot be seen. To perform surgery with adhesions in place, the adhesions, or scar tissue, need to be removed, often away from and involving these vital structures. In the process of removing scar tissue, injury can occur to any structure that is involved with scar tissue. In fact, removal of scar tissue can be much more difficult — and risky — than the procedure itself.
Removal of scar tissue is rarely performed for pain, but can be necessary for those patients with significant pain after surgery that is thought to be related to the formation of scar tissue. General anesthesia is required for the removal of adhesions, and is usually given in association with another procedure, hysterectomy for example, with scarring removed at that time.
Back to TopRemoval of scar tissue is generally a safe surgical procedure. There are cases in which extensive scarring is encountered, with dense thick scarring requiring removal. In some cases, removal of severe adhesions involving the bowel can result in a small hole in the bowel that is usually recognized and repaired. The same is also true of the bladder and other structures in the pelvis.
A serious complication of extensive lysis of adhesions is an unrecognized bowel injury. This is when a small defect in the bowel is not seen and repaired, resulting in bowel contents spilling in the abdominal cavity. The result is “peritonitis,” a severe infection that requires additional surgery and can lead to death. For this reason, surgeons performing extensive lysis of adhesions in the pelvis or abdomen must have experience in the management of adhesions, especially to the bowel, to avoid this dire complication.
Back to TopBecause pelvic adhesions can be tricky to treat, there is always the chance that surgery can exacerbate the problem or cause new adhesions to form. It is therefore important to put your treatment in the hands of an experienced GYN specialist.
The surgeons at CIGC have a niche focus: minimally invasive techniques for GYN surgery that facilitate optimal care and rapid recovery. Gynecological surgery is the only medicine we practice; in contrast, it is only a secondary component of what your OBGYN practices. All of our surgeons have undergone extensive training to become board certified and fellowship trained in minimally invasive technology or gynecological oncology.
Choosing the right specialists for pelvic adhesion removal is an essential part of managing your condition. Many women spend tens of thousands of dollars out-of-pocket for specialist care. At CIGC, we accept most major insurance, allowing our patients to focus fully on getting healthy.
Back to TopIf you think you may have pelvic adhesions, our specialists are ready to provide an evaluation of your symptoms and conditions and recommend an appropriate solution.
Back to Top1 Bolnick A, Bolnick J, Diamond MP. Postoperative adhesions as a consequence of pelvic surgery. J Minim Invasive Gynecol. 2015 May-Jun;22(4):549-63
Schedule a consultation to learn more about how we can treat your condition today.