Fibroids are noncancerous growths that originate from the muscle of the womb and can occur anywhere in the uterus.
For more information about treatments for fibroids, go to treatment options under LAAM Myomectomy or Dualport GYN Hysterectomy.
The most common include Heavy Bleeding and Anemia (low blood count), Pain, Fatigue, Bloating and Distension, Frequency of Urination (pee a lot), Pelvic Pressure and Back Pain.
The best, most comfortable, and least expensive option is Ultrasound.
This is the MAIN reason fibroids grow and cause complications such as heavy bleeding, anemia, pain, and infertility.
For more information on treatment for fibroids, go to Treatment Options under LAAM Myomectomy or Dualport GYN Hysterectomy.
Fibroids can be treated with a variety of methods, from surgical removal to embolization, to other less effective methods.
The BEST option for diagnosis and treatment.
The following section is a more detailed discussion of the summary above. For more information on CIGC HyperSpecialists, the Treatment of Fibroids, as well as information on Publications, Insurance and other issues, please go to the section on Treatment Options – Fibroids.
The most common symptoms of fibroids include heavy bleeding and severe pain during a period, frequency of urination, and infertility.
Fibroids need to be detected and treated early to prevent them from growing larger and causing severe symptoms and infertility.
Pelvic exams – NOT effective. Cannot identify the size, location, and number of fibroids. There are better, more effective methods.
Ultrasound – safe, inexpensive, convenient, well tolerated and accurate, this is the best evaluation of the number, size, and location of fibroids in the uterus.
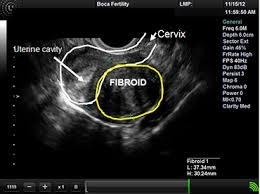
An Ultrasound showing the cervix, the uterine cavity, and a fibroid below the uterine cavity in the muscle of the uterus.
Hysterosonography – also known as a saline infusion sonogram, uses salt water in the uterine cavity at the time of the ultrasound to increase the sonogram’s ability to evaluate fibroids in or near the cavity of the uterus.

Hysterosonogram showing a fibroid in the uterine cavity, with is filled with water.
MRI – compared to an ultrasound, an MRI is a more expensive technique for imaging fibroids, but it is not necessary for the majority of fibroid patients.
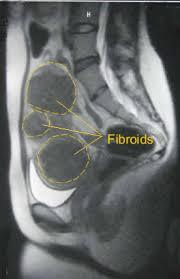
MRI showing multiple fibroids in the uterus
CT Scan – not used for fibroids, there are better tests such as Ultrasound and MRI.
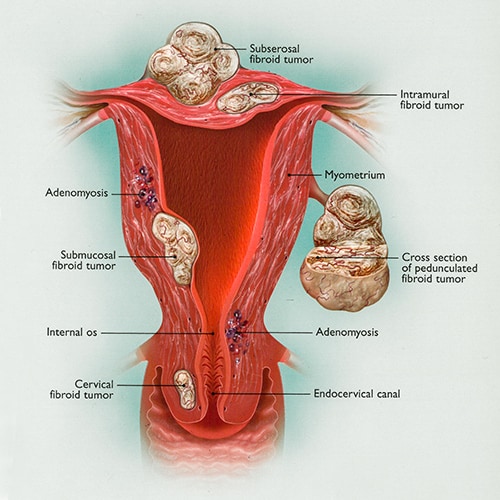
Back to TopFibroids can occur anywhere in or on the uterus and are named for their location.
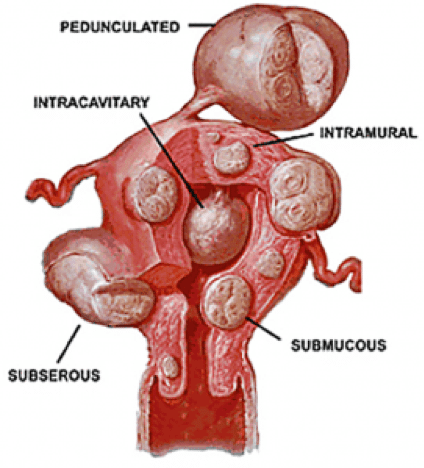
Intramural means “within the muscle” – growing in the uterine muscle wall, or myometrium.
Subserosal fibroids develop on the outside of the uterus and involve the serosal lining of the uterus.
Submucosal fibroids develop under the endometrial lining of the uterus and may protrude into the uterine cavity as they grow.
Pedunculated fibroids develop on stalks attached to the uterus.
The following are common symptoms and complications that occur as fibroids grow.
Anemia is the result of heavy blood loss from fibroids during the cycle, which can cause fatigue, weakness, pale skin, dizziness, headaches and cognitive problems. This condition can quickly turn into a life-threatening situation. Severe anemia can lead to fainting, accidents while driving or at work, stroke, heart attack, and many other problems.
Chronic pain is a common complication of untreated fibroids. In many cases, chronic pain occurs in the pelvic region, but patients may also feel pain in the lower back, abdomen and down the legs. Period pain can be severe in many patients with fibroids and occurs around and during the menstrual cycle. This type of pain can be incapacitating, with many patients unable to work or leave the house.
Infertility occurs when growing fibroids distort the regular shape and function of the uterus.
Bladder compression by fibroids decreases the capacity of the bladder and leads to urinary frequency. Urinary frequency can become a serious problem if a patient is getting up multiple times a night to urinate, causing fatigue from loss of sleep and dysfunction in everyday activities. Fibroids can press on the urethra, the tube that drains the bladder, causing urgency and urinary retention – can’t pee. As fibroids become larger, they can also compress the ureter – the tube that drains urine from the kidney to the bladder. This can cause hydronephrosis, or swelling of the kidney, which can lead to kidney damage.
Abdominal problems can occur, such as distension, bloating, swelling, constipation, and diarrhea. The larger the fibroids, the more serious the problems that occur, leading to abdominal distension. Bloating and swelling results, with many patients looking like they are 20 weeks pregnant or more.
Mental Health and Social Complications from the physical complications of untreated fibroids can be debilitating and negatively impact a person’s quality of life. This can severely affect mental health and lead to higher occurrences of conditions like depression and anxiety. While fibroids and the symptoms they cause cannot be treated by psychotherapy alone, seeking therapy in addition to surgical removal of fibroids can help to support a patient’s mental state when dealing with fibroids and undergoing treatment.
Back to TopThe Hyper-Specialists at CIGC are experts in diagnosing and treating fibroids through advanced minimally invasive surgical procedures. Our experts have performed more than 25,000 GYN surgeries with just two small incisions, no hospital stay and a quick recovery. If you have been diagnosed with fibroids and you’re looking for the most effective treatment option for your case, schedule an appointment today to talk through all available options.
While the true cause of fibroids is still unknown, research is ongoing to find out more. Many potential causes of fibroids are related to both hormones and genetics.
Estrogen
Fibroids are dependent on estrogen to grow. Because ovulation increases the amount of estrogen in the body, hormonal medications like birth control that stop ovulation can also help to decrease estrogen production. Decreasing estrogen production will not stop fibroid growth altogether, but it may help slow down the growth rate in some patients.
Some women are more genetically predisposed to fibroid growth than others. All women are at risk for fibroids, but African American women have fibroids two to three times more than other races. African American women can develop problems at an earlier age, with the tumors growing faster, becoming larger and causing more bleeding and anemia than for women of other races. Patients with a family history of fibroids need special care and counseling to ensure any potential fibroid growth is being closely monitored and, when necessary, treated.
By age 50, about 80% of women will have fibroids. As patients get older, their risk of developing fibroids increases. But for women who are past menopause, their risk declines in accordance with decreasing estrogen production. Routine ultrasounds should be performed regularly to check for fibroid growth. If fibroids are diagnosed, patients should work with a fibroid specialist to explore potential treatment options and keep symptoms under control. This is especially important for patients interested in fertility.
All women are at risk for fibroids, but there are particular risk factors that may have a small impact on the likelihood of developing fibroids. Unlike potential causes, risk factors are often under the control of the patient. Controlling risk factors may not only decrease the chance of developing fibroids, but it can also lead to a healthier life in general.
The following factors may have some relationship to fibroid growth.
If you’re considering a myomectomy or hysterectomy for fibroids, our specialists are ready to provide an evaluation of your symptoms and condition(s) and recommend an appropriate solution.
Back to Top1 Downes E, Sikirica V, Gilabert-Estelles J, et al. The burden of uterine fibroids in five European countries. Eur J Obstet Gynecol Reprod Biol. 2010;152:96-102.
2 Baird D, Dunson D, Hill M, et al. High Cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1): 100-7.
3 Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Human Reproduction Update. 2016;22(6):665-686.
4 Eltoukhi H, Modi M, Weston M. The health disparities of uterine fibroids for African American women: a public health issue.AJOG. 2014;210(3):194-199.
5 Stewart E, Cookson C, Gandolfo R, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501-1512.
6 Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114.
Back to TopSchedule a consultation to learn more about how we can treat your condition today.