Too often, women are only given the option of an open hysterectomy for conditions like large fibroids or an enlarged uterus. Surgical techniques have evolved in the last decade, but the number of women still having open hysterectomy procedures across the United States is unnecessarily staggering.
Back to TopRobotic procedures are becoming more common as hospitals invest nearly $2 million in the machine. While the robot allows surgeons not necessarily trained in laparoscopic procedures to perform more minimally invasive surgery, tools cannot replace skill.
There is no added benefit to the patient, and the surgery can cost, on average, up to $2,000 more than other laparoscopic options and, in some cases, much higher.
Back to TopOpen and robotic hysterectomy procedures are not in the patient’s best interest.
Open procedures, for example, involve:
Similarly, robotic procedures involve:
DID YOU KNOW that advanced minimally invasive hysterectomy procedures for these complex GYN conditions are available?
Discover DualPortGYN—a groundbreaking, minimally invasive GYN surgical technique developed by the our CIGC doctors.
DualPortGYN makes it possible to perform hysterectomies using only 2 tiny incisions—no bigger than a paper cut.
Back to TopDualPortGYN hysterectomy procedures have better outcomes for patients overall.
Let’s review its top benefits:
Additionally, the majority of CIGC patients experience much less pain than women recovering from open or robotic procedures.
Back to TopA hysterectomy for a benign condition is a very personal decision with emotional consequences. Therefore, it should be a decision made by the patient once all the facts are laid out in front of her. A patient should never feel pressured to choose one procedure over another.
Weighing the pros and cons can take time, as there are long-held beliefs about what will happen after removing your uterus.
While many of these are myths, they can create fear and confusion, making the decision even harder. A surgeon must listen closely to a patient’s concerns and explain what happens, what organs are being removed, and how hormones will be affected.
For example, many women are unaware that the ovaries produce the hormones associated with menopause. If left intact, the patient should not experience early menopause and the symptoms of menopause after surgery.
Each woman has her relationship with her body, and doctors must respect their patients and this critical decision.
Back to TopEach patient we have the privilege of serving will receive detailed, in-depth attention from Dr. Natalya Danilyants and Dr. Paul MacKoul. Their renowned personalized care will help you understand your condition and the recommended treatment so that you feel confident from the beginning.
Our surgeons have performed over 20,000 GYN procedures and are constantly finding better ways to improve patient outcomes.
Back to Top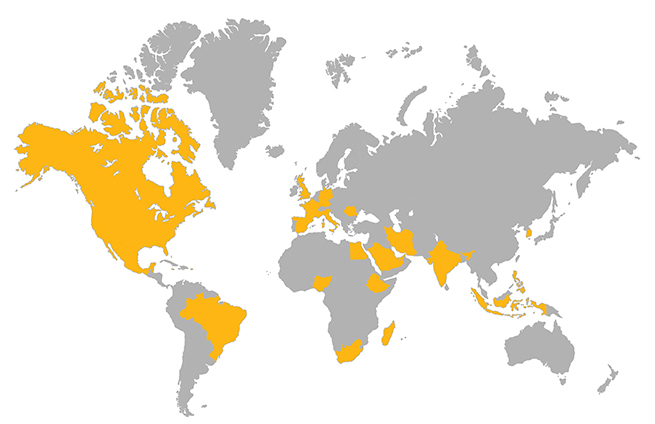
If you are traveling to CIGC from out of the state or country, our Patient Relations Coordinators (PRCs) and Surgical Schedulers will walk you through each step to ensure you are prepared for your arrival.
Learn MoreSchedule a consultation to learn more about how we can treat your condition today.