Ovarian cysts may require removal, especially if cysts are from endometriosis, are causing pain, or are complex and may be cancerous. If surgery is required, realize that there IS a Difference in Laparoscopic Procedures.
CIGC is committed to providing the best possible care for the surgical management of patients with ovarian cysts at the lowest cost. This Value-Based Care model is what sets CIGC apart.
Back to TopMost ovarian cysts resolve on their own because they are normal follicular cysts – a cystic collection of fluid in the ovary that contains an egg. There are many other types of ovarian cysts that can develop and are classified as “simple cysts” which contain just fluid and are usually all benign (not cancer) or “complex cysts” that have solid growths inside or “bands” in the cysts (these are the walls of multiple cysts in one ovary).
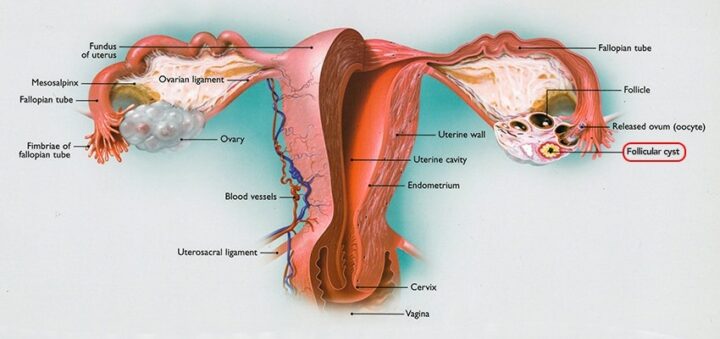
Follicle cysts, seen on the ovary on the right side, are cysts that contain an egg which is released every month. Follicle cysts are normal.
Cysts need treatment if they do not go away, are large, are complex, or cause pain. It is important to make sure that persistent cysts are treated. Cancerous cysts are not common, but early cancers in cysts treated faster will result in much better outcomes than allowing cancers of the ovary to grow and spread. Ovarian cancer is one of the most deadliest of cancers, since it can spread easily to other organs in the abdomen, and has a possible cure rate if treated very early.
Benign (non cancerous) Cysts
At CIGC, laparoscopic surgery is always used to perform either cystectomy (removal of the cyst and keep the ovary) or oophorectomy (removal of the ovary), only if necessary. Regardless of the size of the cyst, almost all benign non cancerous cysts do NOT require an open or robotic procedure when Dualport techniques and procedures are used. This means that a cyst that is 2 cm or 20 cm can be treated laparoscopically with either removal of the cyst only or the cyst and the ovary.
This is very helpful for larger cysts, in which most OBGYNs and Specialists often do large vertical (up and down) incisions to remove the ovary. CIGC techniques allow either the cyst OR the ovary to be removed with a laparoscopic approach allowing for a much faster recovery. Open surgery is not required.
Cancerous Cysts
Ovarian cancer can be treated laparoscopically for many cases of early stage disease. Staging is required – removal of the uterus, tubes, ovaries, lymph nodes, omentum (fat pad off the colon), biopsies and washings. This type of treatment provides a MUCH faster recovery than traditional open surgery, allowing patients to be back to work in 7 – 10 days, with minimal pain, and walking the day of surgery. Laparoscopic staging also allows for patients to start treatment almost immediately after surgery and avoids the two month delay with open surgery.
Advanced ovarian cancer cases are usually treated with open surgery in order to remove all the disease (achieve optimal “debulking”) with better response to chemotherapy.
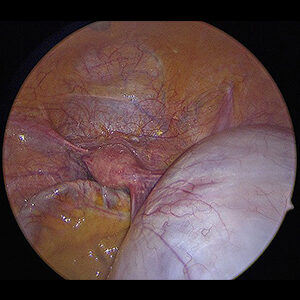
This is a collection of old blood from endometriosis inside a cyst in the ovary. Endometriomas are from the growth of endometriosis on the ovary and can be difficult to remove since in many cases the cysts are difficult to “peel away” from the ovarian tissue.
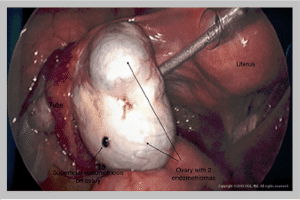
1. Preservation of the Ovary.
A very common problem when OBGYN’s or specialists perform this procedure is removal of part of the ovary when removing the endometrioma or removing the entire ovary. This is not necessary. CIGC uses special techniques and procedures so that almost the entire ovary is preserved during the procedure. A special “orange peel” technique is used, in which the “peel of the orange “– the ovarian tissue – is removed from the endometriotic cyst, the “meat of the orange.” When done properly, even very large cysts can be removed from the ovary with almost all preservation of ovarian tissue. Endometriomas can destroy ovarian tissue over time, resulting in minimal ovarian tissue that is left to be saved. For this reason, all endometriomas should be treated immediately.
2. Endometriomas and Fertility.
Those patients undergoing fertility treatments such as in vitro fertilization or egg freezing should NOT UNDERGO STIMULATION WITH ENDOMETRIOMAS IN PLACE. Unfortunately, some fertility doctors will not send patients to OBGYNs or some specialists for removal BEFORE stimulation due to their concern that a portion of the ovary may be removed due to surgery. Stimulation will increase the growth of the endometrioma, destroy more ovarian tissue, and will cause more pain. CIGC surgeons remove the endometrioma – of almost any size – laparoscopically without loss of a significant portion of the ovary.
Dermoids are the most common type of ovarian cyst, and can have hair, teeth, cartilage, bone, or other glandular (thyroid tissue for example) and skin type elements within. Dermoids are very easy to remove from the ovary. In contrast to endometriomas, they “peel away” very easily with preservation of almost the entire ovary.
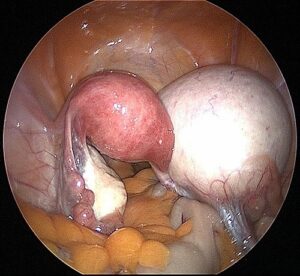
Large Right Dermoid Cyst. In this picture, the Dermoid Cyst is larger than the uterus.
There are many other types of benign cysts that can develop in the ovary, such as serous cysts (serous tissue is like fallopian tube tissue), mucinous cysts (mucus-like), and many others, all of which can be treated laparoscopically. Very large ovarian cysts of any type can be removed with preservation of the ovary in almost all cases with Dualport GYN techniques, so that ovarian removal is not required.
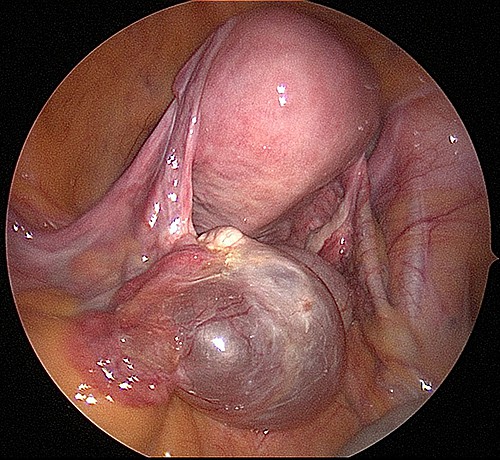
A typical serous cyst, in this case, to the left ovary. These cysts contain clear serous fluid that is thin and water.
Very large mucinous cyst arising from the right ovary. The cyst was too large to fit in the screen and measured at 45+ cm (18″)
All too often, patients are seen at CIGC who are less than 40 years old, want to become pregnant, and had an ovary removed in the past by their OBGYN for a benign cyst. Removal of ovaries is NOT necessary in almost all cases, and will remove half of the eggs present so that fertility will become more difficult. This is especially true if endometriomas or other cysts develop in the remaining ovary. As a patient, please be aware of this, and if your OBGYN or Specialist is discussing ovary removal, consult with a CIGC surgeon for a second opinion.
Older patients close to menopause or those with a history of breast cancer may benefit from removal of the ovary. In these patients, ovarian removal will help prevent the development of ovarian cancer in some cases. For those patients at higher risk of ovarian cancer, removal of the ovary may be the best option. Discussion of your particular situation should be with your CIGC surgeon to determine what the best options are.
Back to TopWatching and waiting is a common treatment plan that OBGYNs use for ovarian cysts. This is a reasonable option for cysts that have just fluid within (simple cysts) and are not complex, which means there are no solid components in the cyst or multiple bands or growths within. For simple cysts, a follow-up ultrasound at 8 weeks is reasonable. If the cyst persists, increases in size, or causes pain, it should be removed from the ovary.
Watching and waiting should NEVER be allowed for endometriomas or complex masses that are concerning for possible malignancy. Allowing endometriomas to grow causes destruction to ovarian tissue and can also create extensive scarring and pain to surrounding organs.
ANY mass that is concerning for ovarian cancer, such as a complex mass with internal growths, needs to be addressed. Watching and waiting is never an acceptable option.
For more information on the HyperSpecialists at CIGC and treatment options for Ovarian Cysts, go to Treatment Options – Ovarian Cysts to find out more.
Back to TopIf you’re suffering with ovarian cysts, our specialists are ready to provide an evaluation of your symptoms and conditions and recommend an appropriate solution.
Back to Top1 Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010 Sep;256(3): 943-54
2 ACOG. Practice Bulletin No 174: Evaluation and management of adnexal masses. Obstet Gynecol. 2016 Nov;128(5):e210-e226
3 Gerber B, Müller H, Külz T, et al. Simple ovarian cysts in premenopausal patients. Int J Gynaecol Obstet. 1997 Apr;57(1):49-55
Back to TopSchedule a consultation to learn more about how we can treat your condition today.