Speak at length to your GYN specialist about your long-term goals and how hormone replacement therapy can play a role in managing menopause symptoms.
Hormone replacement therapy (HRT) is a medical treatment for women that are menopausal, perimenopausal, or postmenopausal that can help relieve symptoms caused by the decrease in estrogen and progesterone. Estrogen is the female hormone that helps minimize or eliminate menopausal symptoms. Typically, menopause occurs in up to 83 percent of women between the ages of 50 and 52, but can occur earlier or later. Hormone replacement therapy can help alleviate symptoms, such as sweating and hot flashes, by balancing estrogen and progesterone in the body.
If you are confused about whether HRT is right for you, you are not alone. The medical community has flip-flopped on this issue over the last few decades and the misinterpretation of data in general media articles creates a feeling of uneasiness for many patients when considering hormone therapy.
Hormone replacement therapy is not one size fits all. The type of therapy, and when it is administered, matters greatly.
Back to TopHormone therapy can be given in two ways1:
Low-dose Vaginal Estrogen Therapy
These products are used to treat vaginal symptoms but do not help with other menopausal symptoms, such as hot flashes, mood changes, or bone loss. They can be taken as a vaginal cream, ring, or vaginal tablet.
Systemic Hormone Therapy
This is what is often referred to as “hormone replacement therapy,” or “HRT.” Systemic means the estrogen is given to you in a form that allows for circulation in the blood stream, and provides a greater overall effect. There are various forms, including oral pills, transdermal patches, or transdermal creams, sprays, or gels. It is important to note that there are two types of systemic hormone therapies: estrogen-only therapy (ET), and combination estrogen and progesterone therapy (EPT). Use of either single-agent estrogen therapy or combined therapy depends on the age of the patient and whether or not the uterus is in place (below).
Hormone replacement therapy, either estrogen-only or combined with progesterone, has been shown in multiple studies to be the most effective treatment available for menopausal symptoms. Estrogen is the most effective treatment available for relief of menopausal symptoms, most importantly hot flashes. In women with a uterus, a combination of both estrogen and progesterone may be a more appropriate treatment, since it is more likely to decrease the risk of endometrial hyperplasia and cancer. Estrogen-only HRT should only be used in menopause if a woman has had a hysterectomy. If symptoms are bothersome, there are several options available.
Some women may derive secondary benefits from taking estrogen-only therapy, including preventing chronic diseases such as coronary heart disease, dementia, or osteoporosis. However, it is not recommended as a first-line medication to address these conditions.
Age is the most important factor when prescribing HRT. The Women’s Health Initiative (WHI) demonstrated that adverse effects with hormone therapy were prevalent in women who were postmenopausal (over age 60). This is not the age group that presents with new onset menopausal symptoms.
Estrogen use in menopause is typically only safe when the uterus has been removed. It is known that estrogen therapy alone, with the uterus in place, will increase the risk of uterine cancer dramatically. Progesterone, the anti-estrogen, can help to avoid the development of uterine cancer, but typically cannot be used with estrogen in menopause since it increases various risks. These risks have been studied extensively in the Women’s Health Initiative (WHI) study, and are discussed below. References have been provided on WHI as well as other studies listed.
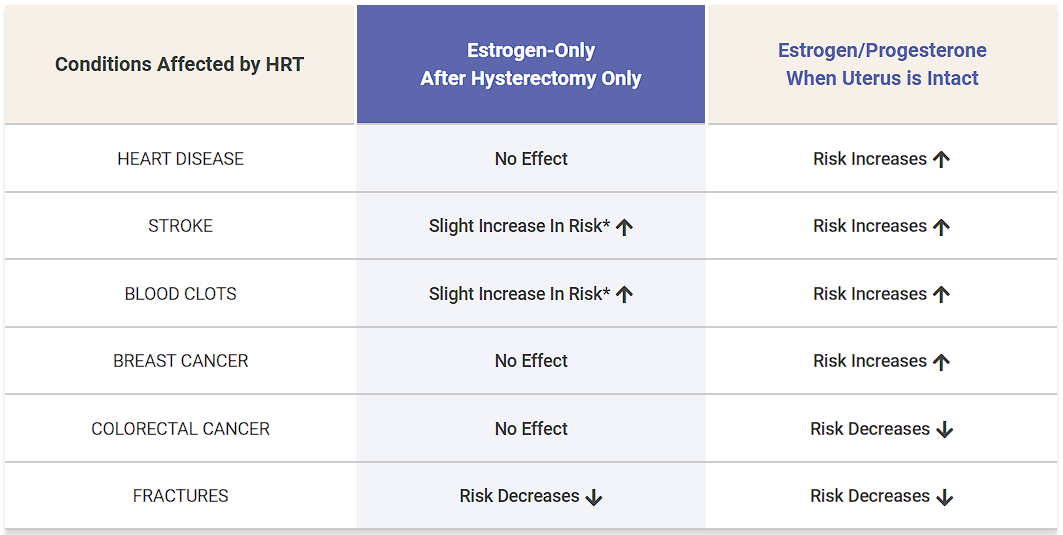
Though there are many benefits, there are also risks of hormone replacement therapy, most notably discovered through a large multicenter study organized by the Women’s Health Initiative (WHI). The risks of HRT include:
* EXTREMELY LOW INCIDENCE
There have been a number of very large, well-designed studies that examined the risks of both types of HRT. Much of the confusion regarding HRT stems from misinterpretation of the WHI.
As summarized on the table above, patients who had their uterus removed can use ET safely with no increased risks of breast cancer, heart disease, colorectal cancer, and decreased fracture risk. There was an extremely low incidence for these patients of stroke and blood clots.
Patients who did not have a hysterectomy using combination estrogen and progesterone therapy had increased risks of breast cancer and heart disease, with decreased incidence of colorectal cancer and fractures. There was an increased risk of stroke and blood clots in this group that was somewhat higher than the ET group.
For patients who have had a hysterectomy and are menopausal, the use of ET is safe and beneficial until the age of 60.
Back to TopWhether a woman enters menopause naturally or surgically, at The Center for Innovative GYN Care® (CIGC®), our GYN surgical specialists have the experience to provide women with tailored hormone replacement therapy when appropriate and understand that each woman experiences menopause differently.
Part of the role of the surgeons at CIGC is to thoroughly evaluate each patient’s unique condition and provide insight to the right approach for therapy. While this may be a form of hormone replacement therapy, it may instead be a series of lifestyle adjustments to cope with the body’s changes.
CIGC surgeons specialize in minimally invasive GYN care. While focused primarily on surgery, additional treatments that support GYN health are critically important to overall patient well-being. Patients who require nonsurgical treatments are offered the best possible medical solutions.
CIGC surgeons are laparoscopic surgical specialists who have dedicated their careers to the performance of minimally invasive GYN care. Additionally, our commitment to surgery means that we have worked on a higher volume of cases, more difficult cases, and use advanced techniques and procedures learned during extensive training. We strive to complete even the most complex surgeries with low complication rates.
We know that our patients are particular when choosing their surgeons, and we think doing extensive research before choosing is important. When you are exploring your hormone replacement therapy options, get to know our surgical specialists and see why they are the best in the industry.
Back to TopIf you’re considering hormone replacement therapy, our specialists are ready to provide an evaluation of your symptoms and conditions and recommend an appropriate solution.
Back to Top1 ACOG Practice Bulletin No. 141: Management of menopausal symptoms. Obstet Gynecol. 2014 Jan;123(1):202-16
2 Santoro N, Epperson CN, Mathews SB. Menopausal symptoms and their management. Endocrinol Metab Clin North Am. 2015 Sep;44(3):497-515
3 Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013 Oct 2;310(13):1353-68
Back to TopSchedule a consultation to learn more about how we can treat your condition today.