Women with interstitial cystitis (pronounced IN-ter-STISH-ul sis-TIE-tis) have a form of painful bladder syndrome. A chronic condition with no known cause, interstitial cystitis can often mimic a urinary tract infection, but antibiotics do not help. Hallmark symptoms include bladder or pelvic pain and the need to urinate urgently and frequently.
The CDC estimates that about 12% of women have early symptoms of the condition. Men can develop it, too, but it is 10 times more likely to show up in women. Interstitial cystitis is not officially a gynecological disorder, but it can co-exist with endometriosis in 60% to 80% of patients. Because of this, and because pelvic pain is also common among women with endometriosis, uterine fibroids and other GYN conditions, CIGC’s specialists evaluate for interstitial cystitis whenever patients are experiencing pelvic pain.
There are limitations, risks and benefits to be found among the many treatment options for interstitial cystitis. It’s important for a woman to consult a GYN expert like those at CIGC who have extensive experience diagnosing this condition and treating mild to moderate cases.
Severe cases may also require the expertise of a urologist or urogynecologist.
If you are experiencing pain and other life-disrupting symptoms of this often overwhelming bladder disorder, the interstitial cystitis specialists at CIGC can help you navigate treatment options ranging from lifestyle adjustments and holistic therapies to medication and surgical procedures. The goal of our specialists is to help you find relief and manage symptoms so you can feel like yourself again.
At CIGC, we understand that each woman experiences bladder disorders differently, and that treatments for interstitial cystitis are not one-size-fit-all. We have helped countless women successfully manage the symptoms and disruption of interstitial cystitis by compassionately and respectfully tailoring therapies to their individual needs.
Back to TopWhile there is no cure for interstitial cystitis, or a single treatment that is effective for everyone, there are numerous self-care, lifestyle and medication treatments worth trying as well as major and minor medical procedures. A specialist can help you explore your options to find what works for you.
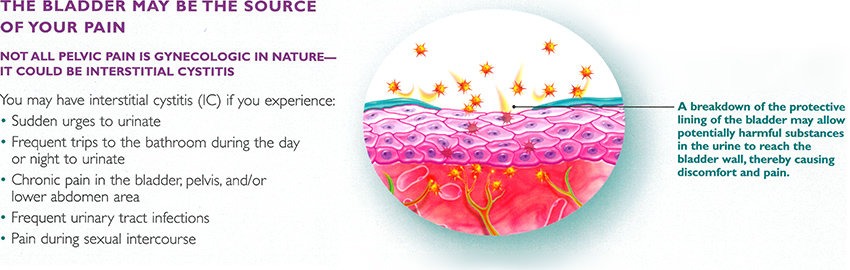
Symptoms of IC include persistent, unpleasant sensations in the bladder, including discomfort with bladder filling, bladder pressure, and bladder spasms. The severity of symptoms can range from mild pressure to severe, debilitating pain. Additional symptoms include urinary frequency, urgency, and frequent urination at night. Seventy-five percent of patients with IC experience pain with intercourse.
Additional symptoms include:
Sexual concerns are common in women with IC. In one study, 90 percent of women with IC reported low sex drive, difficulty with arousal, bladder pain during sex, and urge to urinate during sex.
Back to TopUntreated interstitial cystitis can lead to the following complications:

PETECHIAE, OR BLEEDING SPOTS, OFTEN SEEN AFTER WATER DISSENSION OF THE BLADDER (HYDRODISTENSION). THIS FINDING IS OFTEN SUGGESTIVE OF INTERSTITIAL CYSTITIS.
The goal of a diagnosis is to identify the characteristic features of IC and to exclude other conditions. Diagnosis involves a detailed history of symptoms and associated conditions, a physical exam, and urine testing. IC does not have any characteristic findings on imaging studies. Cystoscopy may sometimes be helpful to exclude other conditions and in patients who do not respond to initial therapy.
Diagnostic methods include:
Abnormal findings on cystoscopy are helpful to support the diagnosis of IC. These findings include reddened lesions (Hunner’s lesions) and small red spots on the lining of the bladder.
Cystoscopy
Under anesthesia, a camera is inserted into the bladder, and the bladder is distended with sterile water (hydrodistention). This procedure allows the doctor to examine the inside of the bladder and perform a biopsy, if necessary. Cystoscopy is often performed with laparoscopy in patients with pelvic pain.
Back to TopIC is a chronic pain syndrome, and there is no treatment that is curative. Treatments that may improve symptoms include lifestyle changes, medications, or procedures. Initial treatment of IC includes dietary changes such as increasing fluid intake and reducing alcohol and caffeine consumption. A second approach will include physical therapy and medications including ibuprofen, pentosan polysulfate, or amitriptyline. Beyond those treatment options, different surgeries may be recommended, such as bladder distention, nerve stimulation, and urinary diversion. There is no consensus on appropriate treatment of IC because the cause of this condition is unknown, the symptoms vary across patients, and there is not enough scientific evidence on the safety and effectiveness of treatments. No treatment has consistently provided relief for all patients. The goal of IC management is to provide relief of symptoms in order to achieve an adequate quality of life.
There are many treatment options for IC, but none are proven to be helpful in all patients. Therapies vary by the risk of adverse reactions and the invasiveness of the treatment. In general, the least invasive therapy is chosen as a first-line therapy. If the symptoms persist, this therapy is discontinued, and another therapy is started. If the symptoms are severe, it may be necessary to proceed rapidly to more aggressive therapies5.
Initial therapy for IC is focused on self-care and changes in lifestyle and behavior to control the symptoms.
Fluid and voiding: Patients who experience worsening of symptoms with concentrated urine should increase fluid intake
Second-line therapy for IC may be time-consuming and usually requires a referral to a specialist.
InterStim is an implantable device that transmits electrical pulses to the sacral nerve located in the lower back. This device has been approved by the FDA for the treatment of urinary urgency and frequency, but not for the treatment of IC.
There is little evidence to suggest that this therapy is effective. This therapy should only be administered by experienced professionals.
This is a surgical procedure and the treatment of last resort. It is reserved for patients whose symptoms significantly affect their quality of life, in whom all other therapies have failed, and for patients who are willing to accept the potential complications and lifestyle changes.
Interstitial cystitis is a common cause of pelvic pain, and in many cases can co-exist with endometriosis in up to 60 – 80% of patients. Since it is often very difficult to isolate IC as a cause for pain, in most patients a pelvic pain work up includes a diagnostic laparoscopy to evaluate and treat endometriosis if present. At the same time, cystoscopy with hydrodistension can be performed to evaluate for IC.
IC is a difficult disease to treat in its moderate to severe forms. Diagnosing the condition is the first step. CIGC surgeons include the evaluation of this condition in the diagnosis of pelvic pain. In many cases, patients with severe Interstitial Cystitis will require the services of a urologist well versed in the treatment of this condition.
Back to TopIf you think you have IC, our specialists are ready to provide an evaluation of your symptoms and condition(s) and recommend an appropriate solution.
Back to TopReferences
1 Bosch PC, Bosch DC. Treating interstitial cystitis/bladder pain syndrome as a chronic disease. Rev Urol. 2014;16(2):83-87
2 Paulson JD, Delgado M. The relationship between interstitial cystitis and endometriosis in patients with chronic pelvic pain. JSLS. 2007 Apr-Jun;11(2):175-81
3 Hanno PM. Interstitial cystitis — epidemiology, diagnostic criteria, clinical markers. Rev Urol. 2002;4(Suppl 1):S3-S8
4 Offiah I, McMahon SB, O’Reilly BA. Interstitial cystitis/bladder pain syndrome: diagnosis and management. Int Urogynecol J. 2013 Aug;24(8):1243-56
5 Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011 Jun;185(6):2162-70
Back to TopSchedule a consultation to learn more about how we can treat your condition today.