Infertility patients should seek out Hyper-Specialists, such as the surgeons at CIGC, for an accurate diagnosis of their condition and the best surgical treatment option available. Dualport and LAAM procedures provide superior options for care over open or robotic surgery, and have fastest recovery with minimal pain after procedures. CIGC results have clearly shown that surgical procedures to optimize the uterus and the ovaries, such as removing fibroids or endometriosis, will increase fertility success rates. This can happen when patients try to become pregnant on their own, or use IVF to assist in pregnancy. CIGC surgical procedures and techniques are outpatient at ambulatory surgery centers, not hospitals, increasing the safety and decreasing the costs of surgery substantially.
The “watch and wait” approach to endometriosis and fibroids is a common OBGYN treatment plan that should not be used for any patient, regardless of their fertility plans. Growth in both of these conditions causes increased pain and associated symptoms and will compromise fertility. Since both fibroids and endometriosis grow through estrogen, and since all patients who are not in menopause produce estrogen, “watching and waiting” allows both fibroids and endometriosis to continually grow. Watching and waiting results in a “DELAY IN CARE” which only causes more problems with infertility over time with these conditions.
Avoid delay in care and progressive infertility. Consult a CIGC surgeon for more information and treatment options that will provide a better chance for fertility now and in the future.
Back to TopThe main causes of infertility include Age, Endometriosis, Fibroids, Adenomyosis, and others.
Age and Declining Fertility
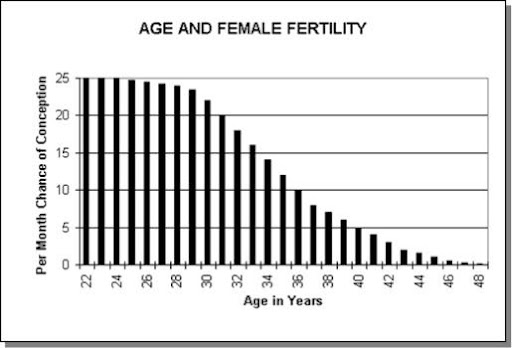
Advancing age is the main cause of infertility in women greater than 35 years old, and becomes the most important factor when considering pregnancy. The following chart shows the “per month chance of becoming pregnant” by age. As can be seen, at age 25 the pregnancy rate every month is 25%, at 35 – 12%, at 40 – 5%, and at 45 – 2%.
So why does infertility decrease with age? The three main reasons:
1. Chromosomal abnormalities in the DNA of eggs.
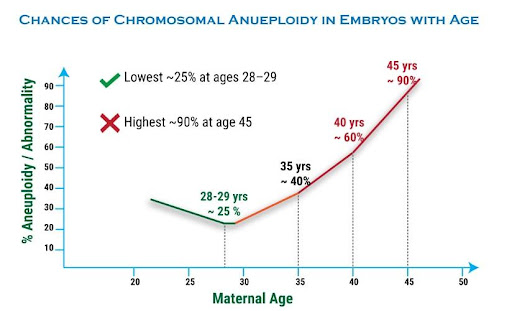
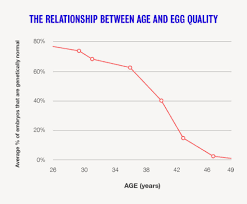
One of the most important reasons is that the chromosomes – or genes – of the egg make more errors in their development as the eggs age. This means that younger patients have more “normal” eggs or better “eqq quality” than older patients. The more normal an egg is, the greater the chance of a normal pregnancy.
Older patients have more “abnormal” eggs and poorer egg quality. The result is that younger patients have a higher fertility rate than older patients.
The first chart below shows increasing chromosomal abnormalities (aneuploidy) in embryos, the egg and sperm combined, as maternal age increases. The second chart shows declining egg quality with age.
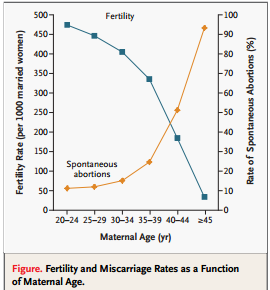
2. Increase in the rate of miscarriage as women get older.
Those same chromosomal abnormalities that occur in eggs and embryos as women age also cause an increase in the rate of miscarriage, or pregnancy loss, with age. Abnormal embryos do not become a pregnancy for a variety of reasons, such as inability to implant into the endometrial lining, or the inability to grow and develop normally into a pregnancy.
The following chart shows the increase in miscarriage – spontaneous abortions – with age.
3. Loss of eggs in the ovary over time.
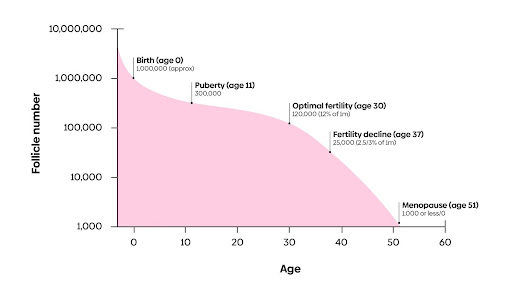
There is a loss of eggs in the ovary over time as women age. This is a natural phenomenon that occurs in all women. With decreasing numbers of eggs available, there is less of a chance to become pregnant.
The following chart shows the number of eggs at every age, with optimal fertility at age 30.
In summary, age and time decrease fertility dramatically, with patients over the age of 40 seeing a significant loss of fertility. How is it possible to assess these factors in someone trying to become pregnant?
AMH – Anti Mullerian Hormone
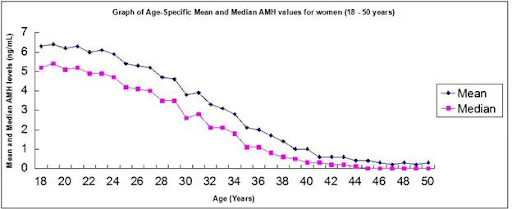
AMH, or Anti Mullerian Hormone, is a substance made in the granulosa cells of ovarian follicles. The follicle is the “capsule” of each egg in the ovary. AMH is a test to identify those eggs that have potential to develop to a pregnancy. The higher the AMH, the greater the “ovarian reserve” or number of eggs a women has that could be available for pregnancy.
AMH does NOT test for egg quality. Egg quality will decrease over time regardless of the AMH level. However, AMH does predict that patients with a higher level will produce more eggs when stimulated with IVF that those patients with a lower level simply because they have more eggs in reserve. This means that a higher AMH may mean a higher success rate in patients under 35. Over 35, egg quality may be a more important factor for predicting fertility rates.
The first chart shows the natural decrease in AMH over time (due to loss of eggs over time.)
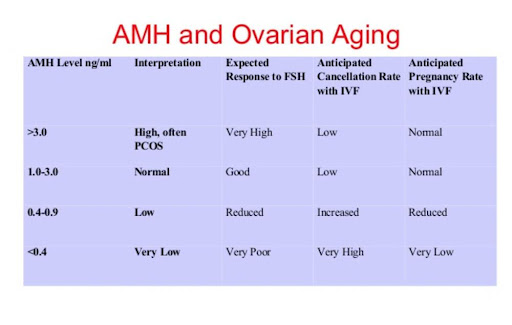
The second chart shows four different sets of information in four columns.
3,4. The “cancellation” of IVF column and “pregnancy rate with IVF” show that success with IVF is decreased with lowering AMH levels. This is because there are less eggs to “mature” towards the formation of an embryo.
IVF – In Vitro Fertilization – is a method that may increase the ability to become pregnant by stimulating the ovaries to produce eggs much faster than normal. Drug stimulation can be used to increase the number of maturing eggs in the ovaries accessible for pregnancy. The eggs are then “retrieved” through an ultrasound procedure and then mixed with the partners sperm to form an embryo – the egg and sperm combined. Embryos are then allowed to develop and grow and can then be “transferred” to the uterus for pregnancy. IVF is a complicated and expensive process, and may or may not be covered by insurance.
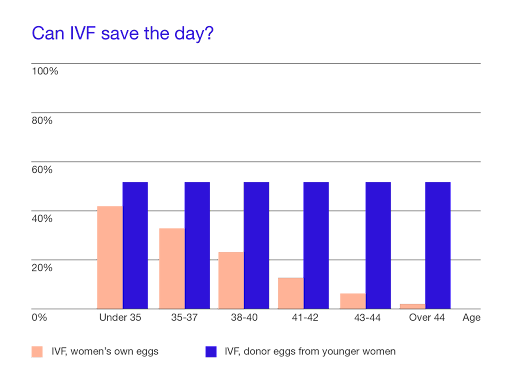
So can IVF save the day? The following graph, from Extend Fertility, clearly shows that IVF has limits in its ability to help with pregnancy. Egg quality is the overriding factor, as can be seen with very low IVF rates in patients over 40. Donor egg IVF is the use of younger eggs from a “donor” to become pregnant. Note the purple bars on the graph indicating that with a donor, the success rates with IVF are very consistent.
There are donor “egg banks” available for patients to review who the donor is, with information all about the donor including their background, education, etc. IVF rates are greatly increased using a donor egg, simply because the egg quality is much better in younger age women. The best donors are between the age of 25 and 32.
Inflammation
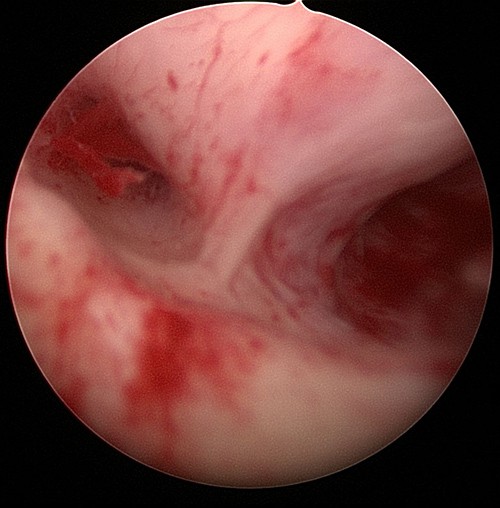
Inflammation from endometriosis is due to implants of endometrial tissue growing and infiltrating (dissecting) into the peritoneal lining. The peritoneal lining covers all organs of the pelvis and abdomen. As the implants (areas of endometriosis) grow into the peritoneal lining, they release inflammatory chemicals that cause INFLAMMATION – a severe reaction which causes white blood cells and other factors to react and try to HEAL the damage. As a result of this injury to affected tissue, PAIN results. As the body tries to heal the damage, SCAR TISSUE can form. Estrogen makes endometriosis grow, so this disease will progress in those women who ovulate or make estrogen.
Inflammation can affect fertility and can:
In the following diagram, red “X”s indicate where endometriosis can block fertility
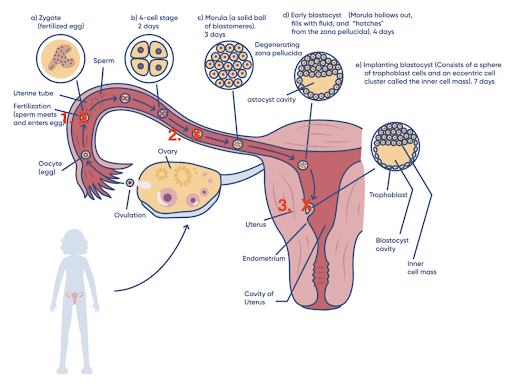
Step 1 – Fertilization
Step 2 – Transport of the Embryo down the tube
Step 3 – Implantation of the embryo into the uterine lining
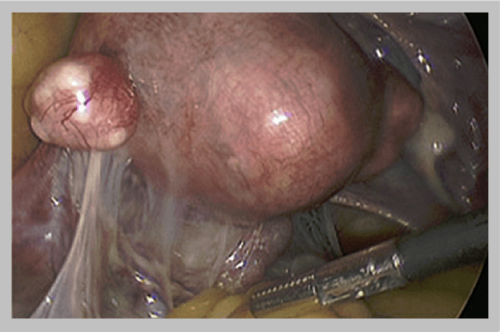
Fibroids are smooth muscle growths in the muscle of the uterus. Two types of fibroids can cause infertility.

Adenomyosis is endometriosis of the muscle of the uterus. This means that the uterine lining – the endometrial lining – grows into the muscle causing pain, bleeding, and inflammation. Since adenomyosis is an inflammatory process just like endometriosis, it will also cause infertility. Inflammation to the muscle is thought to prevent implantation, or growth, of the embryo into the uterine muscle preventing the formation of a placenta and development of the baby.
The cause of adenomyosis is unknown, but is thought to be due to disruption of the “barrier” between the lining of the uterus and the underlying muscle, allowing the adenomyosis to infiltrate or grow into the muscle. The condition is seen more in patients who have had prior uterine surgery. Surgery on the uterus, such as in Cesarean Section, Myomectomy (fibroid removal surgery), or other types of procedures, may displace the endometrial lining cells into the muscle, allowing them to grow and form into adenomyosis. In some patients, there is no history of prior surgery and adenomyosis is still present.
“Focal” adenomyosis is growth in only one area of the uterine muscle, whereas “Diffuse” adenomyosis is throughout the muscle. MRI is the best test to determine if adenomyosis is present, ultrasound and CT scan are not helpful.
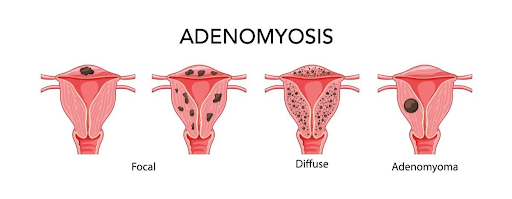
Since adenomyosis can decrease fertility rates in up to 30% of those patients who have it, the diagnosis should be made before any patient starts IVF through MRI. There have been cases in which patients have undiagnosed adenomyosis and have undergone multiple IVF cycles at very high cost unsuccessfully.
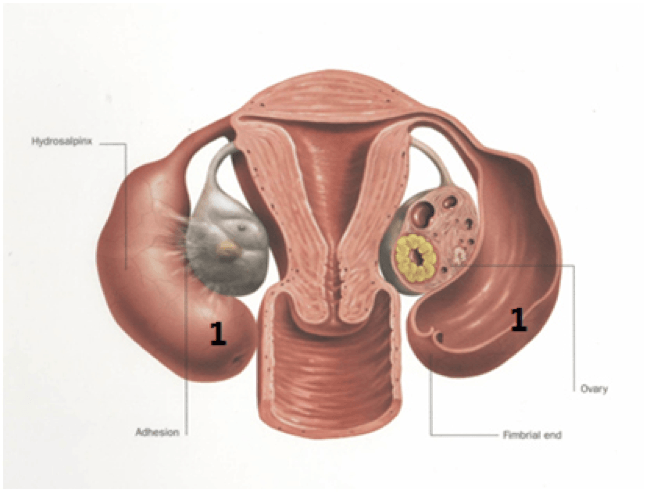
Hydrosalpinx right tube. A right hydrosalpinx – a dilated right tube that is fluid filled, and can decrease fertility.
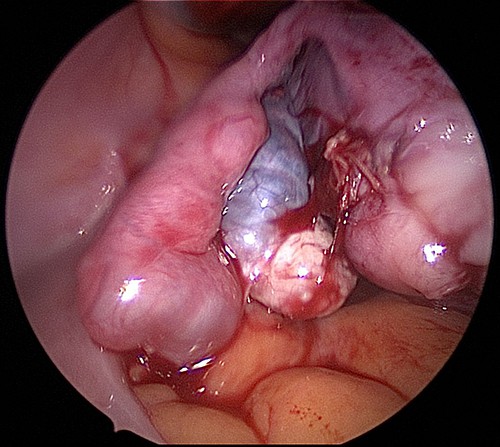
Hydrosalpinx left tube. Left hydrosalpinx secondary to endometriosis
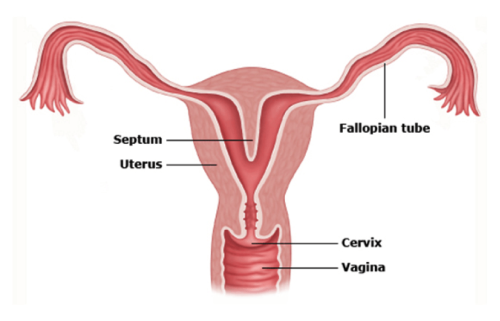
A septum in the uterus dividing the uterus into two separate sections.
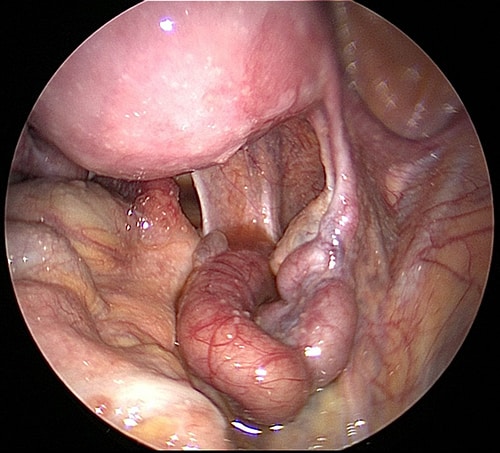
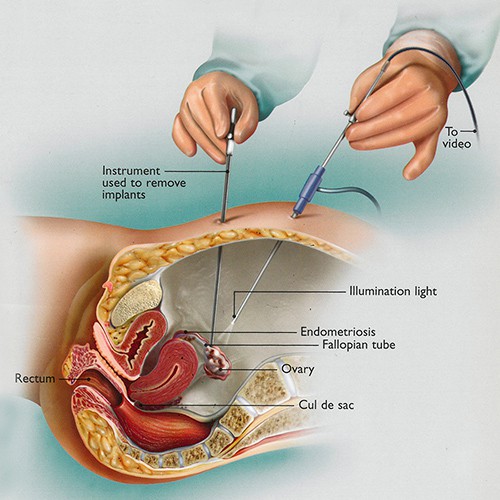
Minimally invasive laparoscopic surgery plays a large role in enhancing treatment success for infertility patients, and may optimize the uterus and the pelvis for invitro fertilization procedures.
For each of the following conditions, please refer to the Treatment Options section for more information. Below is a brief summary of how patients can benefit from a surgical approach for each to enhance fertility.
Endometriosis: Dualport Retroperitoneal Excisional Therapy
Fibroids cause pain and heavy bleeding, and large numbers of fibroids in the uterus can cause inflammation which can also affect fertility. Removal of fibroids through the LAAM procedure has the following benefits.
Fertility
Symptomatic Relief – Removal of fibroids results in dramatic IMMEDIATE benefits for patients, such as:
Recovery – FAST with LAAM procedure, with most patients back to work in 7 to 14 days, not months.
Embolization is blockage of the blood supply of the fibroids through a radiology procedure that does NOT remove fibroids. After embolization, the fibroids remain and may shrink with time. Embolization should NOT be used for the treatment of fibroids in fertility patients. Link out to UFE LP
Hydrosalpinx – meaning “water on the tube” – is when the end of the tube becomes blocked, or obstructed, leading to fluid buildup in the tube.
Causes: Endometriosis, infection, prior surgery, or fibroids can block tubes.
Affect: Toxic fluid builds up in the tube, and can spill back into the uterine cavity and prevent IMPLANTATION of the embryo up to 60% of the time.
Treatment: Removal of the entire tube. This is completed laparoscopically, at which time causes for the blockage can be assessed, such as endometriosis or adhesions, and can be removed. In some cases, lysis of adhesions can remove a blockage while saving the tube.
Adhesions can form from prior surgery, endometriosis, fibroids, infection, and other causes. Blockage of the fallopian tubes is common with extensive scarring, especially from prior myomectomy (fibroid removal surgery) or from endometriosis. Removal of adhesions will help to remove tubal adhesions and restore normal anatomy to the uterus, tubes, and ovaries so that normal fertility function and pregnancy may be possible.
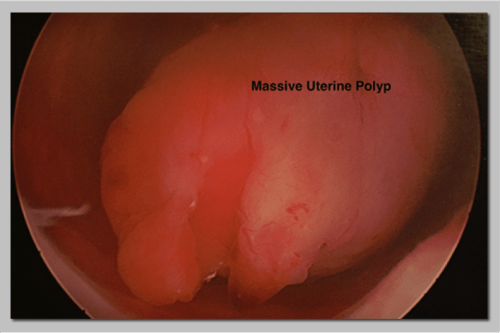
Uterine polyps, submucosal fibroids, intrauterine adhesions, and uterine septum can be removed hysteroscopically – a surgical procedure performed through the cervix on the uterine cavity. Hysteroscopic procedures do not require any incisions, and most women are able to return to work the following day.
Polyps and fibroids can be resected using a resectoscope, and filmy or mild intrauterine adhesions can be cut with hysteroscopic scissors. Extremely dense adhesions are removed using a resectoscope, often with the assistance of a laparoscope to avoid perforation of the uterus.
Intrauterine adhesions can be prevented by using good surgical techniques, minimizing trauma to the uterus and uterine lining, and preventing infection. Following an extensive uterine surgery or resection of intrauterine adhesions, an intrauterine balloon can be placed inside the uterus for approximately seven days to help further prevent adhesion formation. At CIGC, a special “form fitting” balloon is placed inside the uterine cavity that covers the lining better than other types of balloons. This keeps the walls within the uterus from touching each other as they heal, thus preventing them from adhering to each other. High-dose estrogen can be given at the same time to help the uterine lining to proliferate, which also prevents adhesion formation. This is usually taken for one to two months, after which time seven to 10 days’ worth of progesterone is taken to induce a period.

Cook form fitting intrauterine balloon
A second look inside the uterus with the hysteroscope is usually conducted one to two months afterwards. Severe adhesions may require several rounds of this protocol.
Back to TopIf you’re struggling with infertility, our specialists are ready to provide an evaluation of your symptoms and conditions and recommend an appropriate solution.
Back to Top1 Giudice LC. Clinical Practice. Endometriosis. N Engl J Med. 2010 June 24;362(25):2389-98.
2 Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009 Apr;91(4):1215-23
3 Vercellini P, Consonni D, Dridi D, et al. Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Hum Reprod. 2014 May;29(5): 964-77
4 Zhang Y, Sun Y, Guo Y, et al. Salpingectomy and proximal tubal occlusion for hydrosalpinx prior to in vitro fertilization: a meta-analysis of randomized controlled trials. Obstet Gynecol Sur. 2015 Jan;70(1):33-8
5 Harb HM, Ghosh J, Al-Rshoud F, et al. Hydrosalpinx and pregnancy loss: a systematic review and meta-analysis. Reprod Biomed Online. 2019 Mar;38(3): 427-41
6 Pérez‐Medina T, Bajo‐Arenas J, Salazar F, Redondo T, et al. Endometrial polyps and their implication in the pregnancy rates of patients undergoing intrauterine insemination: a prospective, randomized study. Hum Reprod. 2005 Jun;20(6):1632‐5
7 Kodaman PH. Hysteroscopic polypectomy for women undergoing IVF treatment: when is it necessary? Curr Opin Obstet Gynecol. 2016 Jun;28(3):184-90
8 Practice Committee of the American Society for Reproductive Medicine. Uterine septum: a guideline. Fertil Steril. 2016 Sep 1;106(3):530-40
9 Singh SS, Suen MW. Surgery for endometriosis: beyond medical therapies. Fertil Steril. 2017 Mar;107(3):549-54
10 Duffy JM, Arambage K, Correa F, et al. Laparoscopic surgery for endometriosis. Cochrane Database Syst Rev. 2014 Apr 3;(4):CD011031
Back to TopSchedule a consultation to learn more about how we can treat your condition today.