Endometriosis is a GYN condition that happens when tissue from the lining of the uterus – the endometrial lining – grows outside of the uterus to other organs in the pelvis and abdomen. Important points about diagnosing and treating endometriosis:
Pain during and around the cycle is the number one complaint from patients with endometriosis, ranging from mild to incapacitating – so severe that normal activities are impossible. Other symptoms include:
Infertility is a very common result of Endometriosis and can be present in most patients with the disease.
Can only be made by minimally invasive Laparoscopic surgery. Why?
The MAIN reason endometriosis progresses, causes severe pain and fertility and complications is due to a Delay in Care. A delay in the diagnosis and treatment of endometriosis is very common, and is usually due to:
Endometriosis is a “surgically staged” disease. This means that only surgery can determine the “extent” of the disease.
The BEST option for diagnosis and treatment since CGIC Hyperspecialists are GYN Oncology trained and have the highest level of training in surgery.
When endometriosis is not diagnosed quickly and treated properly, symptoms become worse and complications occur. The following is a more detailed discussion of the summary above.
1. Infertility is a common result of endometriosis, even when it is treated properly. Delay in the diagnosis, improper surgical removal, and advanced stage disease are common with endometriosis, leading to severe infertility.
2. Pain can become “debilitating,” meaning that many women cannot go to work or function normally when their cycle occurs. Improper and untimely treatment leads to severe pain, emotional and mental health issues, as well as narcotic use. Pain with intercourse, pelvic pressure and back pain, sharp stabbing pain, and eventually constant pain can occur as the disease progresses.
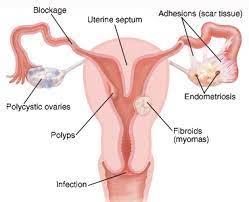
3. Ovarian cysts and Endometriomas can develop with delay in care and late diagnosis.
4. Bowel, Bladder, and other organ involvement can cause problems with pain during bowel movements, urination, and obstruction of the ureters, causing kidney swelling.
5. Inflammation of endometriosis has been linked to immunosuppression, heart disease, and many other negative conditions.
1. Infertility
This can happen at any stage of the disease due to chronic inflammation. In fact, up to 50% of women with endometriosis suffer from infertility. This occurs because the endometrial cells have “mini periods” outside the uterus each month, causing inflammation, pain, and scarring. Inflammation and scarring from endometriosis results in infertility.
2. Inflammation
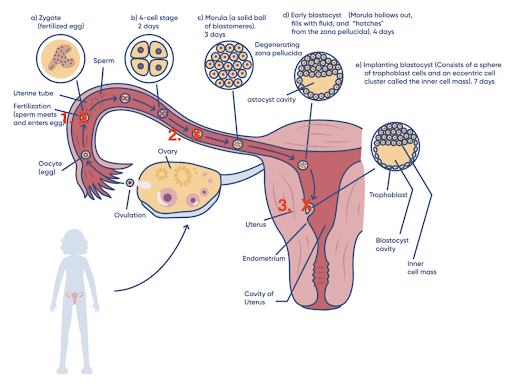
In the following diagram, red “X”s indicate where endometriosis can block fertility.
Step 1 – Fertilization
Step 2 – Transport of the Embryo down the tube
Step 3 – Implantation of the embryo into the uterine lining
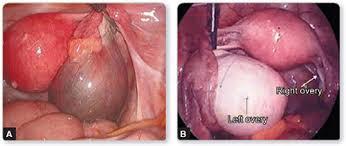
Endometrioma in the right ovary. Endometrioma in the left ovary with normal right ovary.
3. Pain
With endometriosis comes pain from two main causes: Invasion into the peritoneal lining and Adhesions. Delay in treatment creates more pain from this disease, and more complications.

Endometriosis of the peritoneal lining – black and brown implants of disease
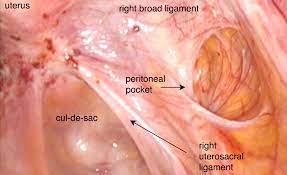
Endometriosis involving the base of the uterus, the pelvis (culdesac) and the peritoneum of the right uterine sidewall
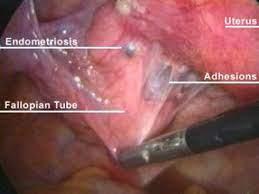
Adhesions between endometriosis, the fallopian tube, and the uterus
4. Ovarian Cysts/Endometriomas
In its later stages, endometriosis can lead to the development of endometriomas – large cystic collections of endometriosis in the ovary. This can destroy and replace normal ovarian tissue, and can lead to decreased ovarian reserve and infertility.
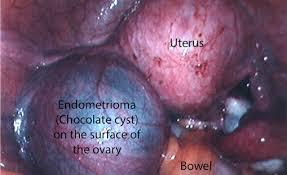
Large endometrioma in the left ovary
5. Bowel Problems- Urinary Problems
Endometriosis can affect the bowel in two ways: it can develop on the outside of the organ (called superficial bowel endometriosis) or penetrate the bowel wall in more severe cases.
In severe cases, deep endometriosis can infiltrate the bowel wall, causing rectal bleeding.

Endometriosis on the bowel
Endometriosis can affect the bladder by growing around and into the bladder wall, causing problems with urination and even blood in the urine. Obstruction of the ureters can result from advanced disease causing kidney swelling and dysfunction.

Endometriosis involving the bowel – left- and the bladder – right.
Studies have shown an increased risk for high cholesterol and coronary heart disease among women with laparoscopically confirmed endometriosis. Due to chronic inflammation and high levels of cholesterol, women, especially young women, with endometriosis may be more likely to develop chest pain, have a heart attack or undergo heart surgery.
Back to TopAn endometriosis specialist can diagnose, stage, and treat the disease through minimally invasive laparoscopic surgery. If you have painful symptoms that you suspect may be caused by endometriosis, early diagnosis will bring you closer to relief
Endometriosis is a condition in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside it. Important points:
Endometriosis is the lining of the uterus – the endometrial lining – going outside the uterus and growing on the peritoneal lining. The peritoneal lining covers all organs of the pelvis and abdomen, and it is where endometriosis grows. The lining has many nerve endings, which sense the growth of endometriosis and its irritation, causing pain.
There are three primary types of endometriosis that all start with growth on the peritoneal lining, and then “invade” or penetrate deeper into the lining with time. Delay in treatment allows endometriosis to grow, so this is why a diagnosis should be made sooner rather than later. All three types of endometriosis can cause pain and infertility.
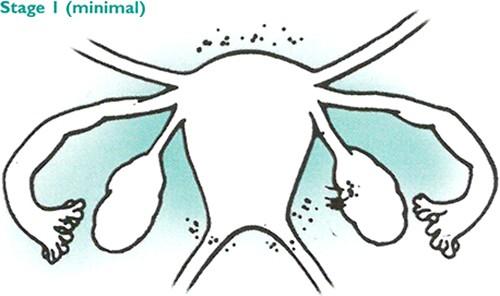
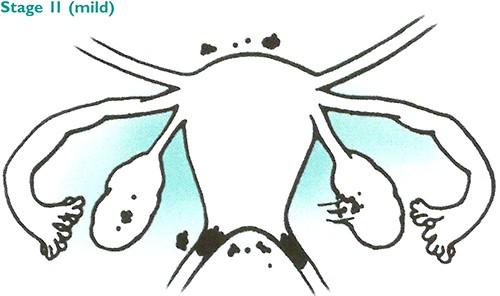
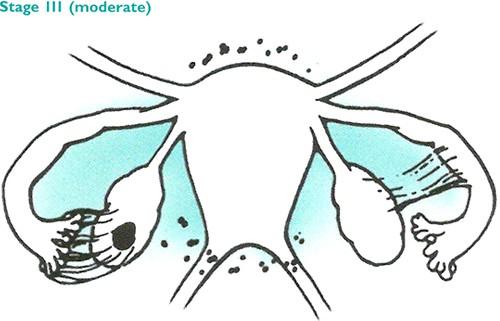
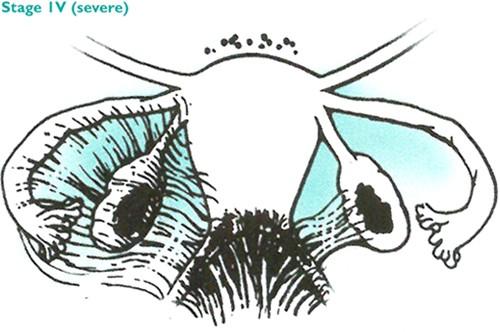
Endometriosis is classified into four stages — minimal, mild, moderate or severe — depending on where the endometriosis is, and how deep it has penetrated into the peritoneal lining.
Stage 1 endometriosis is classified as minimal. In this stage, there are few superficial implants and no significant adhesions or scar tissue. It is still possible to have severe symptoms in this stage despite the light spread of the disease.
Stage 2 endometriosis is classified as mild. In this stage, there can be both superficial and deeper implants, but still without any significant adhesions.
Stage 3 endometriosis is classified as moderate. In this stage, there are multiple deep implants, small cysts on one or both ovaries and filmy adhesions. Adhesions are made up of scar tissue that causes organs to stick together. Adhesions can cause pain and nausea in some cases.
Stage 4 endometriosis is classified as severe. In this stage, there are multiple implants, large cysts on one or both ovaries and dense adhesions. Patients in this stage are at the highest risk of infertility and other complications, so treatment should be considered urgent.
CIGC Hyper-Specialists are NOT OBGYN’s, but are GYN oncology-trained specialists using the powerful DualportGYN RetroPeritoneal Excision method for the surgical removal of endometriosis. The techniques and procedures used by CIGC provide the highest quality of care at the lowest possible cost. Outcomes have shown the fastest recovery and lowest complications.
For more information, please go to the section on Treatment Options, Endometriosis.
Back to TopThe cause of endometriosis is still widely unknown, but there are ongoing studies to determine it, and several likely theories exist on the subject (the most common is a phenomenon called retrograde menstruation). There are also several risk factors that indicate a higher likelihood of endometriosis developing, including short menstrual cycles and never having given birth. It is important to understand these causes and risk factors to understand whether you might be at risk.
While researchers are not sure what definitively causes endometriosis, they have identified several possible causes, including:
Certain factors may place you at higher risk for developing endometriosis. The following are risk factors for endometriosis2:
Choosing the right specialist for endometriosis removal is an essential part of managing the condition. If removed incorrectly or incompletely, endometriosis can continue to cause pain and impact fertility. Our specialists understand what women with endometriosis suffer through, and we put the needs of our patients first. Many women spend tens of thousands of dollars out of pocket for specialist care. At CIGC, we accept most major insurance plans, ensuring our patients can focus on getting healthy.
Back to Top
If you suspect you may have endometriosis, our specialists are ready to evaluate your symptoms and recommend an appropriate solution.
Back to TopSchedule a consultation to learn more about how we can treat your condition today.