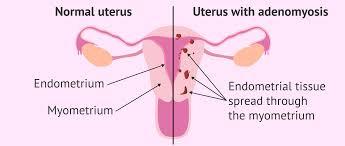
Adenomyosis is a type of endometriosis. Endometriosis occurs when the endometrial lining somehow gets outside of the uterus and grows, thus Endometri (endometrial lining) -osis (outside). Adenomyosis is when the endometrial lining grows into the muscle of the uterus, thus Adeno (glands) myosis (muscle). Once inside the muscle, the endometrial glands grow with each cycle, causing severe pain and bleeding.
Adenomyosis can be difficult to diagnose and is often identified by clinical symptoms – not imaging such as Ultrasound – which cannot identify the disease.
The adenomyosis Hyper-Specialists at The Center for Innovative GYN Care are highly experienced in both diagnosing and treating adenomyosis and can often make the diagnosis by clinical symptoms alone.
The most common symptoms include severe pelvic pain, heavy bleeding, and severe back pain. Pain with intercourse can occur. Anemia and fatigue due to blood loss, leg pain, abdominal distension and bloating.
Ultrasound cannot diagnose endometriosis unless it is more advanced. A pelvic exam and CT scan are not helpful.
Delay in care is common. This is because ultrasounds are normal, and OBGYNs seeing patients with adenomyosis are not experienced in diagnosing and treating this disease. Delay in care results in:
For non-fertility patients, Hysterectomy is the best option.
For Fertility patients, medical therapy to suppress estrogen production is the best short-term option.
HyperSpecialists: The BEST option for diagnosis and treatment. Hyperspecialists are GYN Oncology trained, the highest level of surgical training possible.
HyperSpecialists: Procedures for the Treatment of Adenomyosis
The following section is a more detailed discussion of the summary above. For more information on CIGC Specialists, the Treatment of Adenomyosis, as well as information on Publications, Insurance and other issues, please go to the section on Conditions: CIGC Treatment and choose Adenomyosis.
Adenomyosis occurs when cells that are normally found in the lining of the uterus (endometrium) begin to grow into the muscle of the uterus (myometrium), thickening the uterine wall. Adenomyosis can vary greatly from case to case. It can be Focal (localized in one area of the uterus), Diffuse (involving large areas of the uterine muscle), or develop into a collection of adenomyosis called an Adenomyoma. Adenomyosis can cause debilitating pain and severe menstrual bleeding for some women. However, some women with adenomyosis have no symptoms at all.
Adenomyosis symptoms may include:
Many patients ask about the difference between adenomyosis and endometriosis because the symptoms sometimes resemble each other or occur simultaneously.
The causes of adenomyosis are unknown. More common theories are as follows:
Adenomyosis growth depends on the production of estrogen, so it’s possible for symptoms to resolve after menopause.
Back to TopThe diagnosis of adenomyosis is generally made on a “clinical” basis through the patient’s history and symptoms. A specialist can typically identify adenomyosis as the cause of heavy bleeding and pain.
Adenomyosis can be focal, diffuse, or form an adenomyoma.
MRI Scan
An MRI scan is the best imaging method for diagnosing adenomyosis and can detect the disease up to 80% of the time. MRI shows a “thickened junctional zone” – this is where the endometrial lining is growing into the uterine muscle. This confirms the diagnosis of adenomyosis.
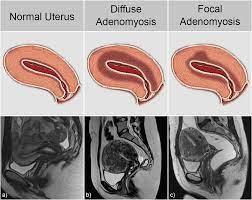
Note the thickening of the junctional zone, which is the uterine lining growing into the muscle.
Ultrasound
An ultrasound can also be used to look for adenomyosis when it is in the advanced stages but is less sensitive than an MRI for early or even moderate-stage disease.
Pelvic Exam
Pelvic exams are not helpful in the diagnosis of adenomyosis.
Post-Hysterectomy Biopsy
The only way to definitively diagnose adenomyosis is by having a pathologist examine the uterus after a hysterectomy has been performed. Looking at the entire uterus under a microscope allows a pathologist to visually confirm the diagnosis.
Missing the diagnosis of Adenomyosis will result in a Delay in Care in the diagnosis and treatment of this disease. Unfortunately, many OBGYNs will miss the diagnosis of adenomyosis more often than not. There are several reasons for this.
Since patients access their OBGYN more commonly than a specialist and often have normal ultrasounds, the disease can be missed, and patients can suffer with progressive and debilitating pain and bleeding. In some cases, an MRI is obtained, which can identify adenomyosis in up to 80% of cases and can be helpful to make the diagnosis by imaging.
If left untreated, adenomyosis may lead to the following long-term complications:
For a full review of Adenomyosis Treatment and the role of CIGC Hyper-Specialists, please go to the section on Treatment Options and click on Adenomyosis.
The only cure for adenomyosis is a hysterectomy.
Any surgical procedure to remove adenomyosis is considered controversial since uterine muscle HAS to be removed if Adenomyosis is removed. Indications:
CIGC surgeons perform LARA in select patients. A consultation is required for qualification and a discussion of risks.
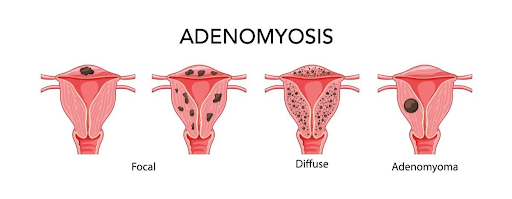
In the above diagram, Focal adenomyosis, far left, can be attempted for removal by surgery since the disease is limited to one area in the uterus. Adenomyomas, a collection of adenomyosis in the muscle far right, can also be removed by surgery. Diffuse disease, second from the right, cannot be removed due to its almost complete involvement of the muscle. Attempts to remove diffuse disease would not remove all the disease or would remove the entire uterine muscle.
For women who are not yet finished with childbearing, the adenomyosis symptoms can be temporarily managed through medication that suppresses estrogen, the hormone responsible for adenomyosis growth.
Some patients may be able to effectively alleviate symptoms like cramping and pelvic pain with NSAIDs like ibuprofen or naproxen. Pain relief using medication is temporary and may only be effective for mild cases of adenomyosis.
Adenomyosis symptoms may also be managed through nonsurgical treatments, including pain management, acupuncture, pelvic floor physical therapy, nutritional counseling and more. These natural and at-home treatments should be advised by a GYN specialist and are not a replacement for essential surgical treatment.
Back to TopAlthough it is most commonly diagnosed in women over 35, it can occur even among teenagers. Current research suggests adenomyosis may be common in younger women as well
Adenomyosis is an extremely common condition, but it is not always readily identified by many doctors. Initial imaging of the uterus is often conducted by an ultrasound, which is commonly used to detect fibroids, but has more difficulty detecting adenomyosis. An MRI scan is a better visual test to detect signs of adenomyosis.
At this time, how adenomyosis affects fertility is unclear. Some studies show an association between adenomyosis and infertility and others show none. In general, it is thought that the severe inflammation caused by migration of the uterine lining into the uterine muscle may prevent implantation of an embryo into the uterine lining.
Many women fear that removing the uterus will immediately send them into menopause and all the symptoms that may accompany it. This is not the case. The ovaries, not the uterus, produce the hormones that dictate menopause. If the ovaries are left in place, a woman will go through menopause naturally.
The only obvious change will be the lack of a monthly menstrual cycle. In many cases, unless there is a genetic risk of ovarian cancer or signs of existing cancer, the ovaries can be retained. Speak to your GYN specialist about your long-term goals and how hormone therapy can play a role in managing symptoms, especially in the transition and early stages of menopause.
No. Although they can occur together, endometriosis is when endometrial cells (the lining of the uterus) are in a location outside of the uterus. Adenomyosis is when these cells are embedded into the uterine wall. Although both can cause pain, endometriosis does not typically cause heavy bleeding.
The GYN Hyper-Specialists at The Center for Innovative GYN Care are GYN Oncology trained – the highest level of training possible. The CIGC state-of-the-art laparoscopic techniques make it possible to treat complex GYN condit/techniques/dualportgyn/”>DualportGYN hysterectomy and LARA procedures are options for patients with this condition and provide the fastest recovery, lowest complication rates, and lowest cost compared to any other surgical option.
Back to TopIf you think you have adenomyosis, our specialists are ready to evaluate your symptoms and conditions and recommend an appropriate solution.
Back to TopSchedule a consultation to learn more about how we can treat your condition today.