By Paul MacKoul, MD - Laparoscopic GYN Surgeon and Co-Founder of CIGC
WHAT ARE Ovarian Cysts & Pelvic Masses
Ovarian cysts are a common occurrence in countless women and often resolve on their own. Many ovarian cysts do not need surgical removal, however cysts that persist may require removal, especially if they cause pain or are suspicious in appearance by ultrasound1,2.
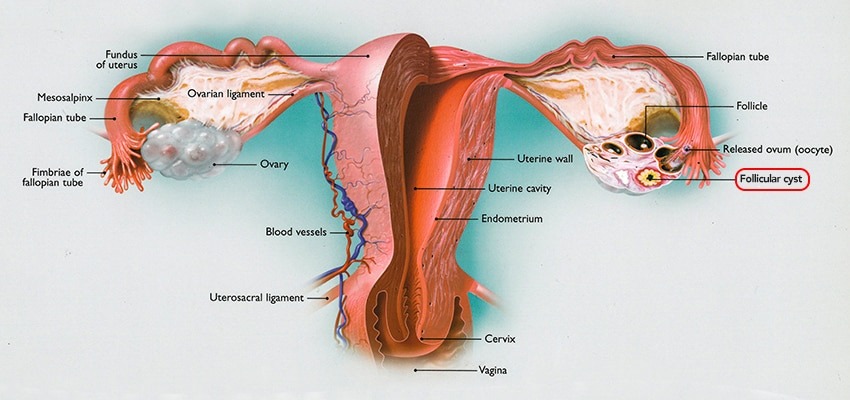
Simple cysts of the ovary are just as they sound — collections of fluid in the ovary without septations, which are bands indicating several cysts in the ovary, or without solid components. These cysts are often just fluid-filled collections that in many cases will resolve on their own. The most common type of simple cyst is a follicular cyst. This type of cyst forms in the ovary every month in which an egg is developing. Sometimes follicular cysts can bleed before or just after ovulation, and are called hemorrhagic cysts. These also often resolve on their own.
Complex cysts of the ovaries have septations present or solid components within and can be either benign or malignant. Benign complex cysts are by far much more common than malignant cysts.
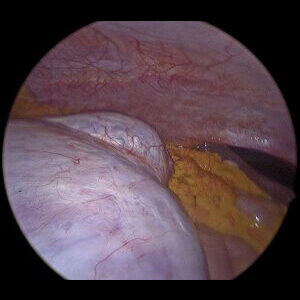
Dermoid cysts are growths within the ovary that can occur at any age, and often contain teeth, skin, hair, and other components.
Mucinous cysts are filled with mucin, which is a thick fluid that sometimes makes these types of cysts very large.
Serous cysts are also very common, and are filled with serous fluid.
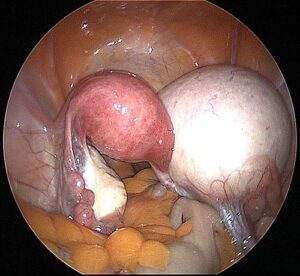
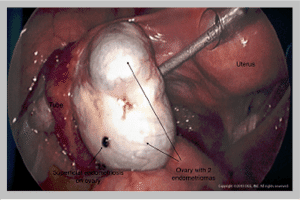
Endometriomas are one of the more common types of cysts, and are collections of endometriotic fluid in the ovary itself. Endometriomas are often referred to as “chocolate cysts” since the fluid is very thick and dark, consistent with old oxidized blood. If left untreated, endometriomas can become very large, and can destroy normal ovarian tissue and cause infertility. For that reason, removal of endometriomas is required to preserve fertility as well as normal ovarian hormone function3.
Malignant cysts of the ovary are rare, and usually occur in patients that are in their mid-40s or older. Ovarian cancer typically has both solid and cystic components, and in many cases has already spread past the ovary to other areas of the body when detected. Most ovarian cancers are epithelial in origin, or from skin cells. Serous cysts and mucinous cysts are the malignant variants of the benign tumors, and their prognosis is mainly determined by the stage at which they present. Stage 1 disease is limited to the ovary; stage 2 to the pelvis; stage 3 to outside the pelvic or lymph nodes; and stage 4 to other areas of the body such as lungs, liver, etc. Most ovarian cancers present as stage 3 disease and require treatment with surgery followed by chemotherapy.
Germ cell tumors are rare types of ovarian cancer that in general have a better prognosis than epithelial cells tumors. Dysgerminoma, endodermal sinus tumors, choriocarcinoma, and others are rare, and often respond very well to surgery and chemotherapy.
Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) occurs due to hormonal imbalance, causing the development of multiple small, benign cysts on the ovaries. This syndrome comes with irregular menstrual cycle, and elevated levels of male hormone causing excess facial and body hair.
Ovarian Cyst Symptoms
Ovarian cysts are typically small and harmless, and do not produce symptoms. However, when they get larger or if they twist, cysts may cause problems. They can rupture and cause internal bleeding, which requires immediate attention and treatment. Women suffering with ovarian cysts may experience any of the following symptoms:
- Menstrual irregularities or abnormal bleeding
- Dull ache in your lower back or thighs
- Pelvic pain shortly before or after the beginning of your menstrual cycle
- Pelvic pain with intercourse (dyspareunia)
- Fullness or heaviness in your abdomen on the side where the cyst is located
- Nausea, vomiting, or bloating from ovary twisting
- Pressure on your bowel or pain during bowel movements
- Difficulty emptying your bladder completely
It is always important to remember that some ovarian cysts may be cancerous. Although very rare in younger women during their reproductive years, the risk of ovarian cancer increases with age.
Additional symptoms include:
- Unexplained weight gain
- Breast tenderness
- Needing to urinate more often
Ovarian Cyst Risk Factors
Risk factors for developing ovarian cysts and pelvic masses include:
- Hormonal problems including drugs that help with ovulation
- Endometriosis which can cause the formation of endometriomas
- Pregnancy which can produce functional cysts
- Sometimes, if a cyst is still present after pregnancy, it needs to be removed
- Pelvic infections which can spread to ovaries and fallopian tubes which cause the formation of cysts
- Previous ovarian cysts
Ovarian Cyst Diagnosis1
Various methods of diagnosing ovarian cysts and pelvic masses are:
- Ultrasound:
Examining an ovarian cyst via ultrasound by looking at the shape, size, and composition, will help determine proper diagnosis and management. A cyst can be fluid-filled, solid, or mixed. Fluid-filled cysts are not likely to be cancerous, while solid or mixed may require further evaluation.
- MRI:
Reserved for solid tumors
- CT Scan:
This imaging test is not very effective for ovarian cysts or imaging of the pelvis — an ultrasound is a better and less expensive test
- Pregnancy Test:
A positive test may indicate the presence of a corpus luteum cyst
- Blood Tests:
A pregnancy test, hormone levels, and a CA-125 test may be necessary, depending on the characteristics of the cyst on the ultrasound — CA-125 tests are often used to evaluate for ovarian cancer
What Does My CA-125 Result Mean?
A CA-125 is a blood test performed to rule out ovarian cancer. As many other benign conditions can lead to an elevated CA-125 level, results are often high in premenopausal women. Conditions such as fibroids, endometriosis, infection, noncancerous ovarian cysts, and others can falsely elevate the value.
OVA1
This is a newer test that is more sensitive than the CA-125, however it has decreased specificity. The higher sensitivity means that OVA1 will detect an ovarian cancer better than the CA-125 when a cancer is present. The decreased specificity means that OVA1 sometimes detects an ovarian cancer when a cancer is not present. This means that some patients with an elevated OVA1 result will actually undergo surgery when a cancer is not present, sometimes with removal of the ovary.
Ovarian Cyst Treatment
In some cases, observation may be all that is necessary, especially for small, functional cysts causing no symptoms. For women who require removal of ovarian cysts or removal of the ovaries, including women seeking prophylactic oophorectomy to reduce future cancer risk, advanced laparoscopic surgery offers fast solutions and nearly painless recovery.
Surgical Treatment Options
Benign (noncancerous) ovarian cysts can usually be removed with laparoscopy, while preserving the ovary. In the case of extremely large masses or endometriomas, the entire ovary and fallopian tube may need to be removed. At The Center for Innovative GYN Care® (CIGC®), patients with very large ovarian cysts can often have the cyst only removed laparoscopically, while preserving the ovary. This type of surgery is highly advanced, and typically is not performed by OBGYNs. Patients desirous of fertility with large endometriomas will often benefit from this type of procedure, since the ovary can be preserved.
Patients seeking cancer prevention due to increased genetic risk factors will also require complete removal of the ovaries and fallopian tubes.
A decision to remove an ovary is based on the patient’s age, the likelihood of cancer, and the safety of the procedure. All patients will have preoperative counseling that ensures they understand options for ovarian preservation or removal. Every effort is made to preserve ovaries for patients who desire fertility. However, patients with suspected cancers, with family or personal history of breast or ovarian cancer, or with prior histories of ovarian pain or scarring may need complete removal of the ovary at the time of surgery.
Patients who are premenopausal, or still making estrogen, will experience premature menopause if both ovaries are removed. In many cases, unless there is a genetic risk of ovarian cancer or signs of existing cancer, the ovaries can be retained. Speak at length to your GYN specialist about your long-term goals and how hormone therapy can play a role in managing menopause symptoms, especially in the transition and early stages.
Surgical Procedure
Typically, one or two tiny (1/4 inch) incisions and one slightly larger (3/4 inch) incision are necessary for a cystectomy or an oophorectomy. The smaller incisions are located at the belly button and on the far right or left side in the bikini line. The larger incision is located just above the pubic bone. Removal of the ovarian cyst or the entire ovary do not differ surgically in terms of surgical time, incisions, recovery, or any other measure. The only difference is whether ovarian tissue is left in place.
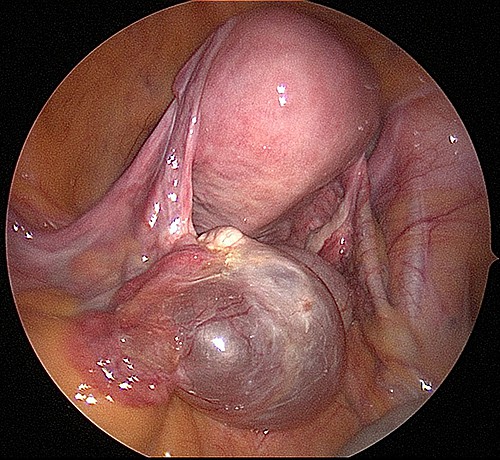
Cysts are surgically removed from the ovary using a unique type of surgical equipment: the harmonic scalpel. This device uses sound waves to cut tissue and seal vessels at the same time. There is a risk that an ovarian cyst may rupture when performing cystectomy. In benign, or nonmalignant cases, this is of no concern. Cysts or ovarian masses that are suspected of being cancerous may require complete removal of the ovary to avoid rupture. While not of immediate danger, if cancerous masses rupture, patients will require chemotherapy due to the spill of cancerous cells in the pelvis.
In order to remove the cyst or ovary from the body safely, a special bag is used to encapsulate the ovary. This allows for easy removal and prevents fluid from the mass from spilling into the pelvic cavity. Any masses suspected for malignancy are sent for frozen section analysis. In frozen section analysis, the mass is sent to the pathologist while the patient is still asleep on the operating room table. The pathologist carefully reviews the sections of the mass to rule out cancer.
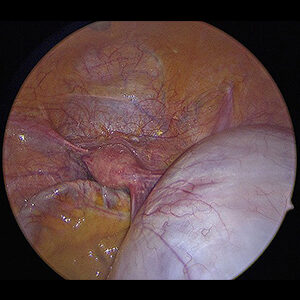
Advantages of Laparoscopic Treatment
Since the vast majority of ovarian cysts and masses in premenopausal patients are benign, laparoscopy is a great option for many patients. Minimally invasive procedures allow patients to avoid large open incisions for the removal of their cysts, thereby decreasing hospital stays, recovery times, and pain. Postmenopausal patients with masses are also usually benign, with cancer rates ranging from five to 20 percent of all masses, depending on the study cited. Laparoscopy is of significant benefit for these patients as well, since it will prevent an open surgery, and recovery from open surgery can be increasingly difficult for older women.
Women who have laparoscopic cystectomy or oophorectomy are almost always discharged from the hospital the same day, with excellent pain control and rapid recovery. Most patients are back to work within seven days.
Ovarian Masses and Cancer
If cancer is identified, a staging operation is performed during the same surgery. Staging means evaluating other areas, such as lymph nodes, to rule out metastasis, or spread of disease, that may require chemotherapy. Laparoscopic staging is more difficult to perform than the open procedure, but allows patients to recover much faster. Cancer patients undergoing this procedure feel better, are stronger, and can start chemotherapy faster with better results by avoiding a two-month recovery. Occasionally, a patient with more extensive malignancy will require open surgery for complete removal of malignant masses, as indicated.
| Laparoscopic Management of Ovarian Cysts and Masses | |
|---|---|
| Indications | All patients without confirmed evidence of ovarian cancer |
| Discharge Home | Same day |
| Recovery Time | Five to seven days |
| Incision Size | One to two 1/4 inch incisions with one 3/4 inch incision |
| Pain Tolerance | Very good to excellent |
| Procedure Time | Less than one hour, range 15 to 60 minutes |
| CA-125 | A hormone marker for ovarian cancer. Can be falsely elevated in premenopausal patients. More accurate in postmenopausal patients. |
| Frozen Section | Performed at the time of surgery to rule out cancer for suspicious masses only. If cancer is identified, staging is accomplished at the same surgical procedure, avoiding a second surgery at a later date |
| Conversion to Open | Rare, usually indicated if ovarian cancer has spread outside of the ovary |
The CIGC Difference
CIGC surgical specialists manage ovarian cysts routinely, and have applied special techniques and procedures to ensure safe and effective results. CIGC state-of-the-art laparoscopic techniques make it possible to treat complex GYN conditions using just two or sometimes three small incisions, with recovery in days, not weeks.
The DualPortGYN® technique was developed by the CIGC minimally invasive GYN specialists to improve the outcomes of GYN surgery. DualPortGYN takes advantage of advanced surgical techniques that enhance the safety of each procedure, allowing the CIGC specialists to perform minimally invasive ovarian cyst removal or removal of the ovary with lower complications, faster recovery, and less pain.
Specialists Not OBGYNs
Many patients have a strong bond with their OBGYN. However, the main focus of an OBGYN is obstetrics, with GYN surgery making up a small percentage of their practice. We partner with OBGYNs to ensure that patients have the best possible care.
It is always better for the patient to have a minimally invasive surgical procedure rather than an invasive open or robotic procedure. At CIGC, our specialists have made a commitment to minimally invasive GYN surgery. We perform a higher volume of cases, see a wider range of case types, and undergo comprehensive training sessions. Surgical expertise is only acquired through performing a high volume of procedures, and since GYN surgery is our main focus, we have developed the advanced skills needed to get patients back to themselves faster, with less pain.
Ready for a Consultation
If you’re suffering with ovarian cysts, our specialists are ready to provide an evaluation of your symptoms and conditions and recommend an appropriate solution.
Related Blog Posts
References:
1 Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010 Sep;256(3): 943-54
2 ACOG. Practice Bulletin No 174: Evaluation and management of adnexal masses. Obstet Gynecol. 2016 Nov;128(5):e210-e226
3 Gerber B, Müller H, Külz T, et al. Simple ovarian cysts in premenopausal patients. Int J Gynaecol Obstet. 1997 Apr;57(1):49-55




