CERVICAL DYSPLASIA
CERVICAL DYSPLASIA AND CERVICAL CANCER
In cervical cancer, the cervix undergoes a transformation known as cervical dysplasia, in which abnormal, or precancerous, cells appear in cervical tissue. The cervix forms the lower, narrow portion of the uterus and leads from the uterus to the vagina. The surface layer of the cervix is mostly composed of squamous cells — these cells are where cancer typically begins to slowly develop. In time, if left undetected and untreated, these cancer cells start to grow and spread more deeply into the cervix and surrounding tissue.

The specialists at The Center for Innovative GYN Care® (CIGC®) know how overwhelming it can be after being diagnosed with cervical cancer. During this difficult time, it is imperative to find a trusted specialist for your treatment. The three types of standard treatment are surgery, radiation therapy, and chemotherapy. Our practice performs advanced, minimally invasive laparoscopic procedures.
Cervical Dysplasia and Cervical Cancer Symptoms
Symptoms of Cervical Dysplasia
Cervical dysplasia is usually asymptomatic since the abnormal cells are only confined to the very top layer of the cervix. This is why the Pap smear is a very important screening test. Additionally, abnormal bleeding can sometimes be a symptom of cervical dysplasia.
Symptoms of Cervical Cancer
In many cases, early-stage cervical cancer does not have any symptoms, which makes the Pap smear a very important test for detection.
- Abnormal bleeding
- Bleeding after intercourse
- Bleeding after menopause
- Vaginal discharge
- Pain during sexual intercourse
- Pelvic and back pain
- Pelvic or abdominal pain (advanced stage)
- Blood in urine (advanced stage)
- Blood in stool (advanced stage)
- Weight loss (advanced stage)
- Fatigue (advanced stage)
- Leg pain or swelling (advanced stage)
- Leakage of urine and feces from vagina (advanced stage)
- Bone fractures (advanced stage)
Cervical Dysplasia and Cervical Cancer Causes1
HPV, or the Human Papillomavirus (see below section on Cervical Cancer and HPV)
- Immunosuppressant drugs
- HIV
- Smoking
- Smokers are twice as likely as nonsmokers to develop the disease
Risk factors for cervical dysplasia include the contraction of HPV, which may be caused by:
- Being sexually active before the age of 16
- Having multiple sex partners
- Having a partner who has had multiple sex partners
- Having sex with uncircumcised men
Cervical Dysplasia and Cervical Cancer Diagnosis
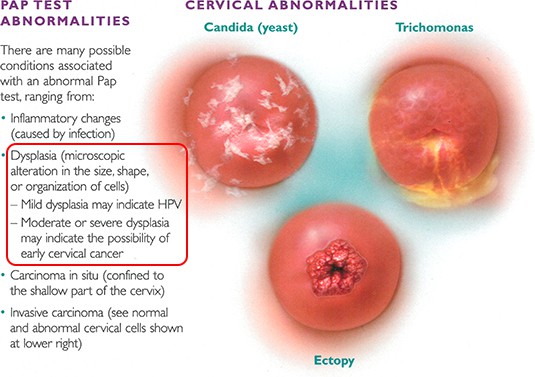
Doctors who provide care for women routinely perform pelvic examinations and Pap smears to screen for cervical cancer in the cells on the surface of the cervix. During a Pap smear, a sample of cells from the cervix is taken and examined under a microscope. Abnormal results from a routine Pap smear should not be cause for alarm. Approximately 6 percent of all annual Pap smears will produce an abnormal result, and this result rarely indicates the presence of cervical cancer. Abnormal cells may suggest, however, that changes leading to cancer are occurring, which is why additional testing may be advised.
Abnormal Pap Smear/Treatment of Cervical Precancerous Lesions
If physicians feel more information is needed following an abnormal Pap smear, further evaluation can be performed using a lighted microscope (colposcope) to better visualize the cervix or to perform a biopsy. If the biopsy is normal or shows only mildly abnormal cells (low-grade dysplasia), no surgical treatment is necessary. Most of the mildly abnormal cells go away on their own and should be followed up with Pap smears to confirm resolution. If the biopsy shows moderate or severe dysplasia, surgical treatment is usually required. A conization, or cone biopsy, removes a cone-shaped sample of tissue from the cervix. This procedure, known as LEEP, which stands for Loop Electrosurgical Excision Procedure, can be performed in the office without sedation or in the operating room under sedation. If it still remains unclear whether the abnormal cells are confined to the cervix or arise from inside the uterus, a dilation and curettage (D&C) may be recommended. During a D&C, a small sample of the uterine lining (the endometrium) is taken from the inside of the uterus.
Treatment of cervical cancer during pregnancy depends on the stage of the cancer and the stage of the pregnancy. For early-stage cervical cancer or for cancer found during the last trimester of pregnancy, treatment may be delayed until after the baby is born.
Cervical Cancer
As with other cancers, cervical cancer is described in terms of its presence in and beyond the cervix. The stage of the cancer describes the extent to which it has spread beyond the cervix, if at all.
The Stages of Cervical Cancer are2:
HPV & Cervical Cancer
Certain strains of HPV have been found to cause cervical cancer. These strains are called high-risk HPV. HPV 16 and HPV 18 are the most common high-risk strains that cause cervical cancer3. When these high-risk strains are detected in a Pap smear, colposcopy is necessary to evaluate the cervix for abnormal cells. If no abnormal cells are found, no treatment is necessary because, in most cases, the infection is cleared spontaneously. Most sexually active women will have HPV at some point during their lifetimes; however, only a fraction will develop cervical cancer. Regular follow-ups with Pap smear screenings allow for early diagnosis of precancerous cells and avoids progression to cervical cancer. In the United States, the rate of cervical cancer is dramatically lower than in countries where the Pap smear is not routinely performed.
Cervical Dysplasia and Cervical Cancer Treatments
Surgery is commonly used as the treatment for cervical cancer. The type of surgical procedure that is needed depends upon the stage and grade of cervical cancer. Small, highly localized areas of precancerous cells or early stages of cervical cancer may be treated with cryosurgery, LEEP, or cold knife cone biopsy (CKC). Some of these minor surgical procedures can be performed in the office.
Types of Surgery for Cervical Cancer:
- Cryosurgery uses an instrument to freeze and destroy a small area of precancerous cells
- LEEP can be used for slightly more invasive cells, because it uses a thin wire loop to cut away a small area of tissue
- CKC can also be used to remove a small area of precancerous or cancerous cells
- CKC is effective for lesions within the opening of the cervix or cervical canal
Hysterectomy
For cervical cancer that is not localized to the cervix or for patients who do not wish to preserve future fertility, hysterectomy is typically the best treatment. Hysterectomy, which is the removal of the uterus and cervix, prevents a recurrence of cervical cancer.
Laparoscopic hysterectomy offers women all of the benefits of minimally invasive surgery, including little to no hospital stay, minimal pain, and fast recovery. A fast and easy recovery from surgery benefits cancer patients in particular because women feel less sick after laparoscopic surgery, which enables a brighter, more optimistic outlook. This positive outlook helps women through the rest of the cancer treatment and recovery process.
Laparoscopic modified radical hysterectomy (LMRH) is a revolutionary procedure for the surgical management of early-stage cervical cancer. This is a technically difficult procedure that — in experienced hands — yields excellent results with much improved recovery and function. During an LMRH, the uterus and cervix are removed, and the tissue on the sides of the cervix is removed as well. To do this, the ureter, or the tube that transports urine from the kidney to the bladder, must be carefully separated from the tissue surrounding the cervix, so that the potentially cancerous tissue can be removed without harming the ureter. This is the most difficult part of the operation. Ureter complications, including nicks and cuts, are the most common type of surgical complications with the LMRH and any other gynecologic surgery.
Staging is performed at the time of the laparoscopic procedure to determine if the cancer has spread, and involves node dissection, or the removal of the lymph nodes during the procedure. The removal of lymph nodes does not add time or additional complications to the surgical procedure. The advanced laparoscopic techniques allow our surgeons to completely isolate the ureter from the surrounding tissue and safely remove potentially cancerous tissue without harming the ureter and other essential structures. All patients with early-stage cervical cancer are candidates for this surgical procedure.
The CIGC Difference
As a patient who has been diagnosed with dysplasia or cancer of the cervix, uterus, or ovaries, it is important to find a GYN surgeon you trust. Surgeons at CIGC are laparoscopic surgical specialists who have dedicated their careers to the performance of minimally invasive GYN surgery.
Our commitment to surgery means that we have worked on a higher volume of cases, more difficult cases, and use advanced techniques and procedures learned during extensive training. We strive to complete even the most complex surgeries with low complication rates.
Surgery is the only medicine practiced by our surgical specialists. Increased surgical volume is important to develop and maintain surgical expertise, and with dysplasia and cancer, a minimally invasive specialist who focuses solely on surgery is essential.
CIGC surgeons do not perform open hysterectomies on patients with dysplasia and cancer. Open surgeries are known to be painful, have a relatively high risk of complications, and have an extended recovery period. CIGC surgeons also do not perform robotic surgeries. Surgeries in which robotic technology performs the procedure are extremely expensive and have a high risk of complications. At CIGC, we perform minimally invasive, advanced laparoscopic hysterectomies using our advanced DualPortGYN® technique. This type of hysterectomy is far superior as it leaves you with minimal cosmetic scarring, has a recovery period of only a few days, and has a low risk of complications. Hear why our patients prefer our laparoscopic procedures.
Specialists Not OBGYNs
Patients who have laparoscopic surgery have little to no hospital stay, minimal pain, and a fast recovery. Since recovery is so easy and fast, patients feel less sick afterward, which contributes greatly to an optimistic outlook. Feeling better physically and mentally makes the rest of the cancer treatment and recovery process more tolerable. At the end of treatment, patients get to walk away with minimal scarring.
Know your options. The surgeons at CIGC assess our dysplasia and cancer patients on a case-by-case basis in order to choose the best treatment options. We partner with OBGYNs to ensure patients have the best possible care. There are many different types of treatment options, and the type of surgical procedure needed depends on the stage and grade of cancer. CIGC will offer you peace of mind by understanding your condition and options.
Cervical Dysplasia FAQs
Ready for a Consultation
If you think you have cervical dysplasia or cervical cancer, our specialists are ready to provide an evaluation of your symptoms and condition(s) and recommend an appropriate solution.
Related Blog Posts
References:
1 Cervical cancer screening and prevention. Practice Bulletin No. 168. American College of Obstetricians and Gynecologists. Gynecol. 2016;128:e111–30.
2 PDQ® Adult Treatment Editorial Board. PDQ Cervical Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated 03.01.2019. Available at: https://www.cancer.gov/types/cervical/patient/cervical-treatment-pdq.
3Crosbie E, Einstein M, Franceschi S. Human papillomavirus and cervical cancer. Lancet. 2013;382(9895):889-99


