LEARN MORE ABOUT FIBROIDS
WHAT ARE UTERINE FIBROIDS?
At the Center for Innovative GYN Care (CIGC), highly skilled specialists use advanced techniques and procedures to provide the best option for all patients with fibroids. Those patients seeking fertility treatment should undergo fibroid removal through surgery, and not by other noninvasive techniques such as embolization and MRI guided ultrasound, to avoid complications that can affect pregnancy such as uterine damage and early miscarriage.
CIGC offers the most effective fibroid removal surgery procedures for fertility patients needing myomectomy using LAAM procedures, and DualPortGYN hysterectomy for women who have completed childbearing. At CIGC®, we take into consideration your future family planning goals and desired treatment options. We provide personalized care to every patient to ensure they are getting the treatment that is right for them.
On This Page
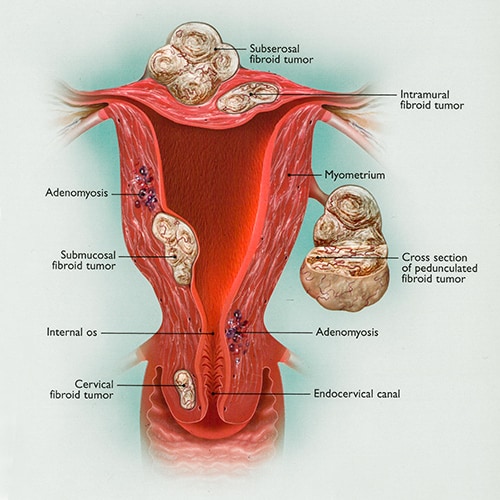
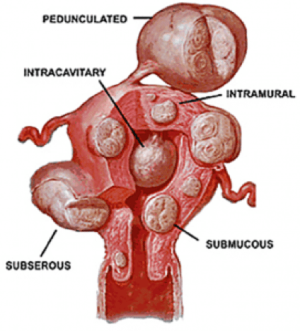
Fibroid Types
Fibroids can occur anywhere in and around the uterus and are named for their location. Cervical growths are considered rare, as most fibroids develop from the muscle of the uterus, or myometrium.
Fibroid Causes
While the true cause of fibroids is still unknown, research is ongoing to find out more. Many potential causes of fibroids are related to both hormones and genetics.
Fibroid Symptoms
Fibroids don’t always present with symptoms, but when they do, the most common symptoms include heavy bleeding, severe pain with the menstrual cycle and infertility.
Fibroid Diagnosis
An accurate diagnosis is crucial for detecting and treating fibroids. The earlier the diagnosis, the better because small fibroids will grow to become larger fibroids that can cause more severe symptoms and increase the risk of complications over time. Pelvic exams are not the most effective diagnosis method for fibroids, so it’s recommended that patients always ask their doctor for an ultrasound.
Fibroid Complications
If allowed to grow, fibroids can have serious complications. These complications may include anemia (which can be life-threatening), infertility, higher risk of premature birth, twisting of fibroids or bowel and urinary tract issues.
Fibroid Risk Factors
Fibroid Treatments
Fibroid treatment is usually surgical, medical or radiological. Recommended surgical treatment includes a hysterectomy (removal of the uterus) or myomectomy (removal of fibroids while keeping the uterus intact). Medical treatment includes hormonal medications like birth control or other medications that reduce estrogen production and inflammation. Radiological treatments include uterine fibroid embolization, MRI-guided ultrasound and radiofrequency ablation, though these treatments are not recommended by CIGC.
If fibroids are causing debilitating symptoms and interfering with quality of life, surgical removal may be necessary to find complete relief. The surgical specialists at CIGC meet with fibroid patients to evaluate each individual case and recommend an appropriate treatment plan.
Fibroids FAQ
What is the best treatment for fibroids?
There are many treatments for fibroids, but in general for those patients who desire to become pregnant, fibroid removal by surgery — also known as myomectomy — is the preferred option. Removal of the fibroids allows for the bulk of the fibroids to be removed and gets the uterus back to normal in most cases to allow for pregnancy. As fibroids become larger, however, the risks of fibroid removal increase. For fertility patients, these risks include scarring to the cavity of the uterus and tubes, as well as abnormal healing leading to infertility. Other options such as embolization, radiofrequency ablation (Acessa), MRI-guided ultrasound, and others that do not remove the fibroids should not be considered. These techniques may decrease the size of the fibroids but may also cause problems such as an increased incidence of miscarriage as well as difficulty in becoming pregnant or maintaining a pregnancy.
Do fibroids cause weight gain?
Only in cases of very large fibroids. Even the largest fibroids have a maximum weight of five to 10 pounds. Fibroids are bulky, but do not weigh a lot. A five-pound fibroid, for example, may be as large as a small watermelon.
Is it possible to naturally get rid of fibroids?
No. Fibroids grow through estrogen production, which occurs throughout a woman’s life until menopause. At menopause, estrogen production stops, and fibroids can shrink. It is important to note that fibroids never completely go away. A large fibroid may only decrease in size by one half after menopause, and this may take years. Fibroids can also undergo “degeneration” after menopause and loss of blood supply. Calcific degeneration, for example, “calcifies” the fibroids, turning them into very hard masses that are difficult to remove. This is a common form of degeneration for fibroids and can cause significant discomfort.
What size of fibroid requires surgery?
Removal of fibroids depends on location, symptoms, and the desire for fertility. A 1 cm fibroid — about one half an inch — can cause severe bleeding if it is in the uterine cavity and can also cause infertility. Fibroids this size should be removed. The same fibroid in the muscle or outside of the uterus does not require removal. Larger fibroids should be removed, since fibroids rarely stay the same size, but continue to grow as long as estrogen is being made (i.e., before menopause occurs).
Fibroid Specialists at CIGC
For the best chance at effective relief from fibroid symptoms, seek treatment from a proven fibroids specialist. A specialist with a high level of expertise in treating fibroids will lower complication rates and risks of incomplete fibroid treatment. The fibroids specialists at CIGC use advanced laparoscopic techniques that put patients’ well-being first. Both the DualPortGYN® and LAAM® procedures involve only two small incisions and a quick recovery. Using state-of-the-art ambulatory surgery centers, each procedure is performed on an outpatient basis so patients can go home the same day.
The CIGC Difference
The Center for Innovative GYN Care techniques are exclusive to our practice. DualPortGYN ® and LAAM ® (laparoscopic assisted abdominal myomectomy) were developed by the CIGC minimally invasive GYN specialists to improve the outcomes of GYN surgery. DualPortGYN and LAAM take advantage of advanced techniques that enhance the safety of each procedure. These procedures have drastically reduced surgery time, decreased the number and size of incisions and identified optimum placement of the incisions, all of which lead to reduced recovery time and pain.
Ready for a Consultation
If you’re considering a myomectomy or hysterectomy for fibroids, our specialists are ready to provide an evaluation of your symptoms and condition(s) and recommend an appropriate solution.
Related Blog Posts
References:
1 Downes E, Sikirica V, Gilabert-Estelles J, et al. The burden of uterine fibroids in five European countries. Eur J Obstet Gynecol Reprod Biol. 2010;152:96-102.
2 Baird D, Dunson D, Hill M, et al. High Cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1): 100-7.
3 Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Human Reproduction Update. 2016;22(6):665-686.
4 Eltoukhi H, Modi M, Weston M. The health disparities of uterine fibroids for African American women: a public health issue.AJOG. 2014;210(3):194-199.
5 Stewart E, Cookson C, Gandolfo R, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501-1512.
6 Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114.