NO PATIENT DESERVES THE RELENTLESS PAIN OF ENDOMETRIOSIS, No Matter How Strong
CIGC Hyper-Specialists Will Help You Take Control of This Disease
THERE IS NO BETTER OPTION
Top 6 Reasons CIGC is the Better Option
(def: An Extreme Specialist, working in a particularly narrow and specialized field)
- GYN Oncology trained surgeons at the highest level of training
- There is No Better Surgeon for this disease: NOT the OBGYN, the minimally invasive GYN specialist, the General Surgeon or Urologist
- The most effective form of Excisional treatment available
- In one 30 minute surgery, Hyper-Specialists accomplish what Orlissa or Birth Control pills will NEVER achieve.
- Medical therapy does NOT
- Prove superior outcomes
- Superior quality care, lowest possible cost
CIGC Hyper-Specialists and Endometriosis – the most effective, safe, and affordable treatment possible.
A 30 minute consult with a CIGC surgeon will provide insight into what endometriosis is and how it should be treated. From diagnosis, surgical treatment, medical suppression and fertility advice all while using your in-network insurance benefits – CIGC Hyper-Specialists are the better option.
Emily's Story: Minimally Invasive Endometriosis Removal
Top 6 Reasons Explained
CIGC specialists are experts in the diagnosis and surgical management of endometriosis. They have performed more than 25,000 surgical procedures to treat complex conditions like endometriosis, and have dedicated their careers to providing the best possible treatment for this difficult disease.
Hyper-Specialist: GYN Oncology trained surgeons at the highest level of training who concentrate ONLY on surgery, not Obstetrics, providing patients the best possible care and outcome.
- GYN Oncology training uses very advanced techniques for the removal of cancers, which include surgery on the bowel, bladder, ureters, vessels, diaphragms
- Endometriosis is NOT a cancer but spreads locally much like cancer and is surgically treated the same way
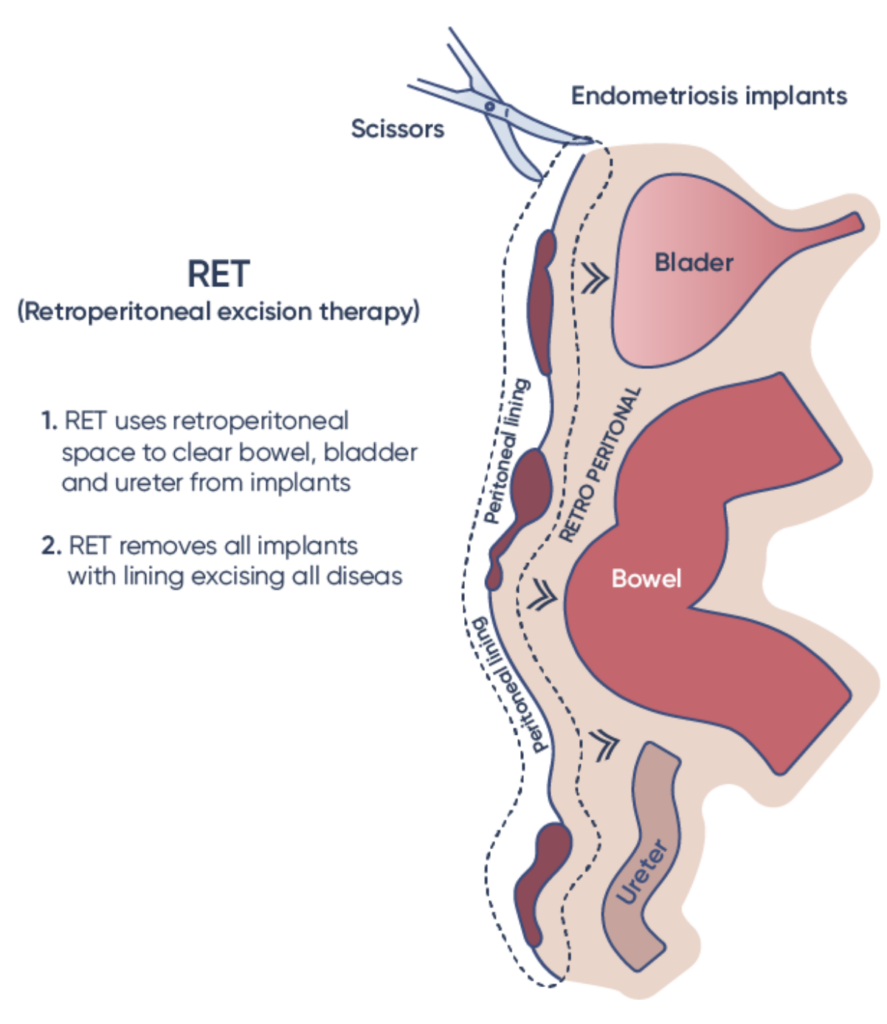
- Using advanced GYN Oncology cancer techniques such as DualportGYN Retroperitoneal Excisional Therapy (RET) provides the best endometriosis care possible
- OBGYN’s and Minimally Invasive endometriosis “specialists” are typically NOT trained in these advanced techniques, and often do NOT remove all disease OR “ablate” (burn) endometriosis implants, which is not nearly as effective
Dualport RET for Endometriosis: THE BEST possible surgery performed in a rapid time frame with very low complications and high success rates.
- DualportGYN uses a combination of two to three incisions cosmetically placed and Retroperitoneal Excision Therapy (RET) to ensure the best possible outcomes for any GYN condition
- The results are dramatic: immediate relief of pain, removal of ALL disease which decreases inflammation and increases fertility rates
- Robotics are NOT required
- CICG NEVER uses ablation or burning techniques which do not remove all disease and are not effective
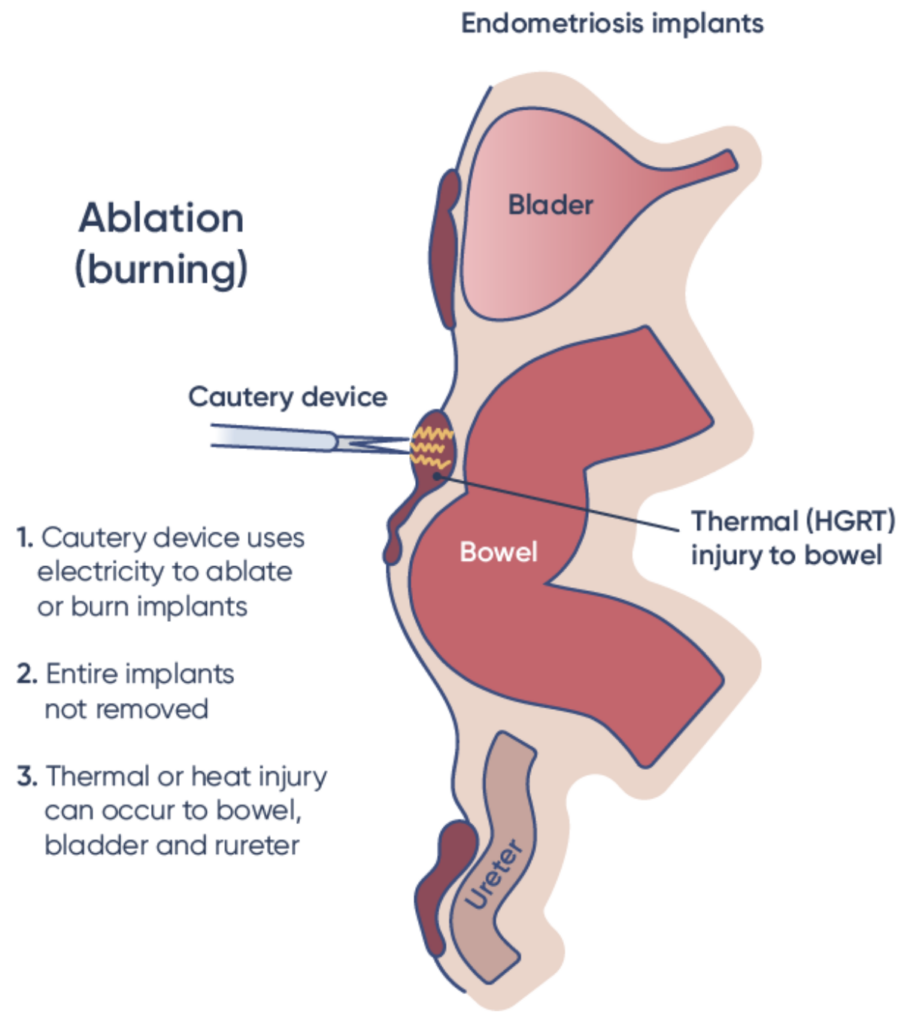
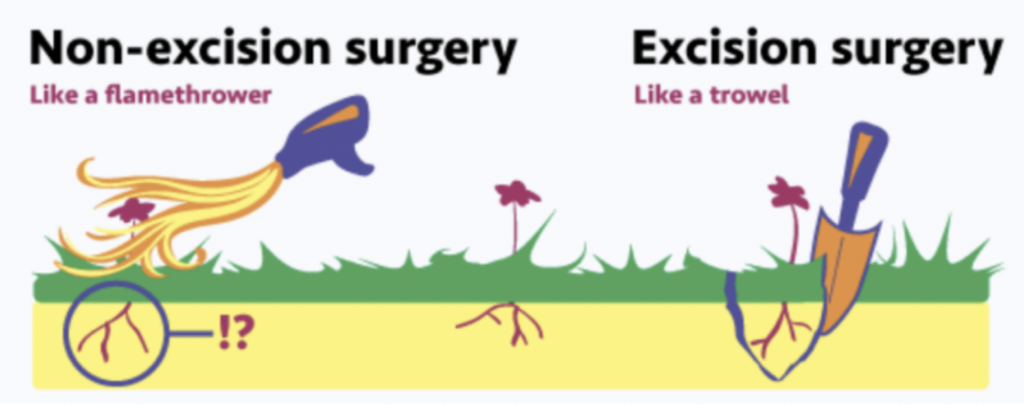
Ablation (burning) vs. Excision
Source: “The Endo-Graphic” by Sarah Soward
RET is a highly advanced technique that allows the removal of ALL disease from any structure in the pelvis or abdomen. Since endometriosis involves the peritoneal lining covering all organs, RET separates out the lining from the organ, and then goes retro – or “behind” the lining – to remove all the disease safely and quickly to any structure. That includes not only endometriosis on the tubes, uterus, and ovaries, but also on the bowel, bladder, ureters (tubes that drain urine from the kidney to the bladder), diaphragm, and other structures.
Surgery is ALWAYS performed first – the reasons why:
- Surgery STAGES the disease and tells how advanced it is so the correct medical suppression can be used AFTER surgery
- Surgery removes ALL the disease when RET is used, and does in 30 minutes what it would take medical therapy MONTHS or NEVER to achieve
- Surgery immediately treats pain and symptoms. Medical therapy takes much longer, and inadequately treats the disease
- Surgery does not have menopausal side effects that last for months with Orlissa or Lupron therapy, or weight gain with other stronger medicines
- Surgery potentially can INCREASE fertility rates after removal of disease
- Medical therapy DECREASES fertility rates for an extended time after starting treatment
- This is because medical therapy stops OVULATION, which decreases estrogen. Estrogen makes endometriosis grow. No ovulation, no pregnancy.
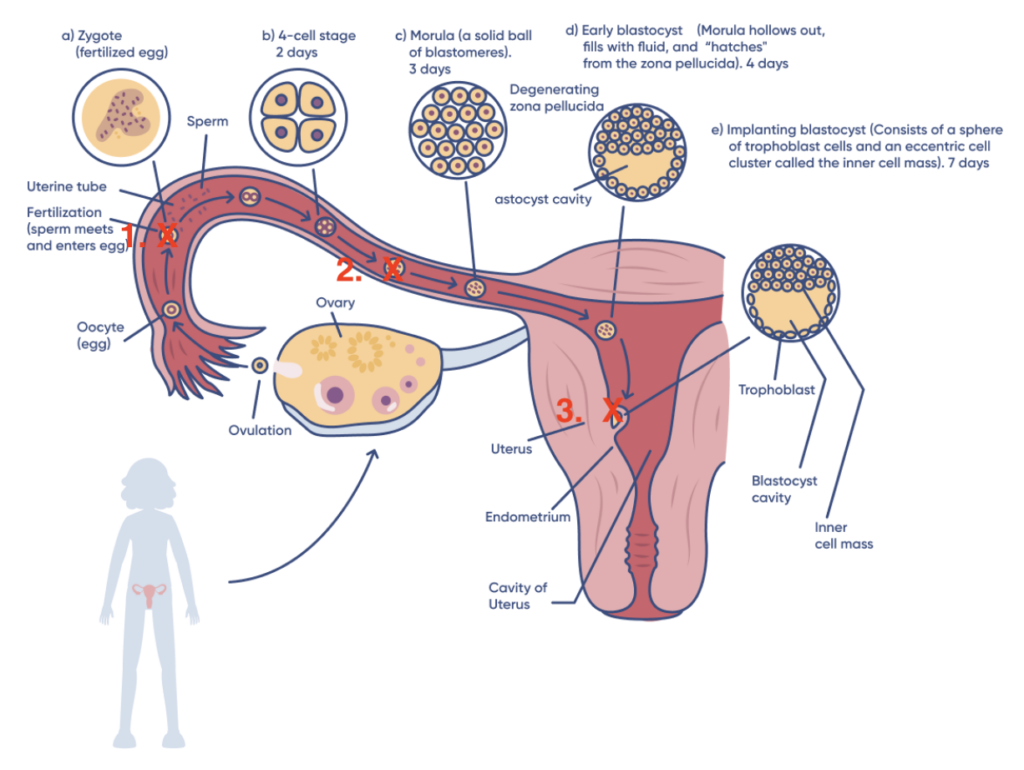
Endometriosis causes inflammation, which decreases fertility.
Inflammation:
- Blocks the formation of the sperm and egg to form an embryo
- Prevents the embryo from traveling down the fallopian tube to the uterine cavity
- Decreases implantation of the embryo into the uterine lining to form a baby
Endometriosis excision:
- Removes endometriosis and scar tissue from the tubes
- Decreases inflammation to allow for embryo implantation
- Significantly enhances fertility
- In the following diagram, red “X”s indicate where endometriosis can block fertility
Successful endometriosis surgery can increase fertility chances when surgery is properly performed with removal of all disease since inflammation is decreased. Symptoms of severe pelvic pain, difficulty with intercourse and pain with intercourse, heavy bleeding, and the need for narcotics to control pain can resolve after surgery as well.
- Dedication and devotion to surgery is what CIGC is all about. That allows CIGC surgeons to perform a high volume of surgical procedures that allows refinement of techniques and procedures, and increases success while decreasing complications.
- High volume surgeons will ALWAYS have better results than low volume surgeons
- CIGC publishes those results in “peer reviewed journals” which educates the public and other health care providers about CIGC results and outcomes
¹ A Retroperitoneal Approach to Endometriosis Excisions: Surgical Outcomes and Seven Year Followup
² Prevalence and Risk Factors of Coexisting Endometriosis in Women Undergoing LAAM for Symptomatic Leiomyoma and Subfertility
- CIGC surgeons are NOT Cash Based OR Out of Network – they do NOT require payment up front in the tens of thousands of dollars to provide care
- CIGC participates with most insurance plans AND provides care equal to, and often better than, Cash Based or Out of Network surgeons
- CIGC surgeons use qualified Surgery Centers to perform surgery. Customized care in a comfortable, convenient surgery center increases the quality of care while further reducing the costs and the inconvenience of the hospital.
- CIGC does not use Robotics. Robots are hospital based, use more and larger incisions, are more expensive with much higher complication rates, and are not needed to provide the highest quality of care.
There is NO BETTER OPTION
The result is SUPERIOR QUALITY CARE while using your IN NETWORK insurance to keep your costs as low as possible. Endometriosis does not discriminate between the wealthy and the not so wealthy. Neither should your surgeon.
Speak With Our Team
A member of our patient care team would be happy to walk you through what to expect, answer your questions and help you get started with your treatment process.
CIGC Hyper-Specialists and Surgery Centers
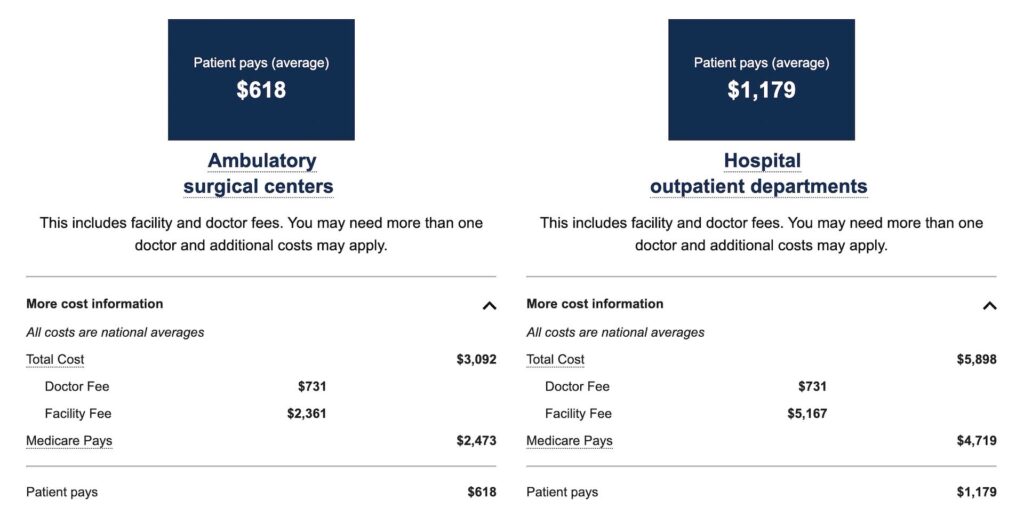
CIGC surgeons perform DualportGYN Retroperitoneal Excision Therapy in their own approved GYN focused ambulatory surgery centers. Surgery in an outpatient surgery center is safer with higher patient satisfaction than a hospital, and at much lower cost. This is “Value Based Care” – the best possible care at the lowest possible cost.
The following is from Price Procedure LookUp from Medicare.gov, and shows differences in pricing between ambulatory surgery centers and the hospital for a laparoscopic code for removal of endometriosis. The code below is just for one procedure – often several codes are used so there is an even greater savings. The information below is an example and is not representative of what patients will pay. Each patient’s cost will vary according to their insurance cost share, but overall surgery centers will decrease costs dramatically over the hospital.
Laparoscopy, surgical; with fulguration or excision of lesions of the ovary, pelvic viscera, or peritoneal surface by any method. Code: 58662
Consult with a CIGC Hyper-Specialist
Consider a consulation with a CIGC Hyper-Specialist to discuss options available for you and your particular needs. In a 30 minute session, CIGC will customize a treatment plan that will outline differences in surgical and non-surgical options, and how DualportGYN Hysterectomy can help you improve your quality of life and emotional health. CIGC is the leader in minimally invasive GYN surgery, and will always provide information to you that has your best options in mind.
Our Patients Say it Best: What Life is Like After Endometriosis Excision

“After surgery at CIGC I could tell this time was different. I had surgery on a Thursday, rested on Friday, and on Saturday I was up and doing normal stuff. Now I feel like I could run a mile. I feel so light now. All of my activities, work, elder care, none of that feels as heavy anymore. Nothing is slowing me down.”
– Dorran

“I had a negative experience with a past laparoscopy and made CIGC aware. This experience was nothing like the last. I felt heard, comfortable, safe and well informed. The staff and facility are top notch!”
– Terri
Are You Looking for an “Endometriosis Specialist Near Me”?
CIGC is an advanced center for endometriosis treatment where you can speak with a dedicated endometriosis specialist to find the best possible solution for your condition. Contact us today to get your life back on track.
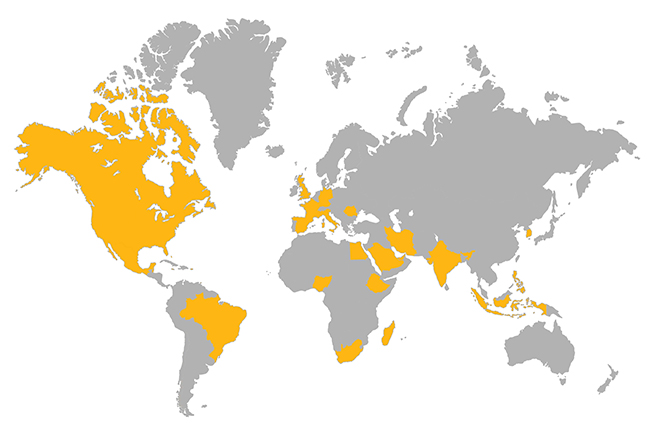
Superior Surgical Outcomes Published in Top Medical Journals
The DualPortGYN procedure has been proven superior to other minimally invasive techniques and open surgery. In addition, we have shown that these procedures can be performed safely and more efficiently in an ambulatory surgery center. Our nationally and internationally renowned techniques have been published in prestigious medical journals due to exceptional patient outcomes.

Worldwide Destination for GYN Care
Our Locations

Rockville, MD
Office Location
3206 Tower Oaks Blvd,
Ste 200
Rockville, MD, 20852

Reston, VA
Office Location
1860 Town Center Dr,
Ste 255
Reston, VA, 20190

Clifton, NJ
Office Location
975 Clifton Ave
Ste 202
Clifton, NJ 07013

CMS – Secaucus, NJ
Surgical Center
210 Meadowlands Pkwy
Ste 5
Secaucus, NJ 07094

ISC – Rockville, MD
Surgical Center
3206 Tower Oaks Blvd,
Ste 100
Rockville, MD, 20852

